Diagnostic Operations
Find your care
Call 310-825-5111 to learn more about our world-class pediatric neurosurgery services.
What are the different types of diagnostic operations (invasive EEG monitoring) for epilepsy?
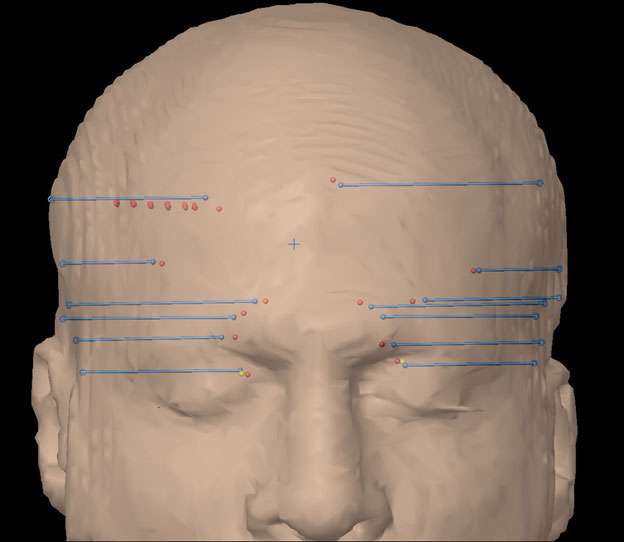
There are 2 main types of surgical procedures to identify the area of the brain from where the seizures originate. This includes a subdural grid electrode evaluation, which allows physicians to record brain activity from the surface of the brain, and a depth electrode evaluation, which allows physicians to record brain activity from the depth of the brain. Both options can allow the epilepsy team to precisely determine the area of seizure onset with extreme precision. For either operation, special equipment is used in the operating room to precisely place these electrodes in predetermined locations as planned by the epilepsy team. A postoperative CT scan is also performed to confirm the final position of each electrode prior to recordings of the brain activity.
How is a subdural grid electrode implant procedure performed?
Once the patient is placed under general anesthesia, an incision will be made and a piece of the skull will be lifted up that will be replaced at the end of the surgery. Through this opening, a thin plastic grid will be placed directly on the surface of the brain and the wires will be tunneled under the scalp through a separate area. A neurologist will perform short term monitoring in the operating room to ensure that we are recording high quality signals from the electrodes. The scalp is then closed and the patient is woken up from anesthesia prior to obtaining a CT scan and later transferred to the pediatric intensive care unit for further monitoring of the brain activity.
How is a depth electrode implant procedure performed?
Once the patient is placed under general anesthesia, several very small incisions are made on the scalp through each of which, a thin electrode (about the width of a spaghetti noodle) is passed into deep structures of the brain. Short term monitoring is performed in the operating room with the help of a neurologist to ensure that we are recording high quality signals from the electrodes. The patient is then woken up from anesthesia prior to obtaining a CT scan and later transferred to the pediatric intensive care unit for further monitoring. Pain from this procedure is minimal, as the scalp and skull do not need to be opened.
Who is a good candidate for invasive EEG monitoring?
In general, patients are considered to be a good candidate for an invasive EEG evaluation if the MRI is normal, there is uncertainty as to where the seizures are originating in the brain or the presumed area where the seizures are originating are close to potentially important functional areas of the brain.
How many days is invasive EEG monitoring typically performed for?
Invasive EEG monitoring is usually performed until we have recorded at least 3 to 4 of the patient’s typical seizures and we have performed brain mapping through cortical stimulation. It is difficult to predict how long this will take for each individual patient. The majority of patients spend 3 to 4 days in hospital while they undergo invasive EEG monitoring.
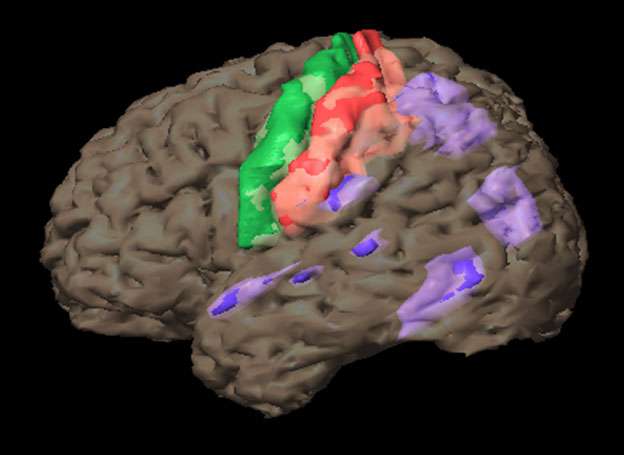
How is brain mapping performed?

Brain mapping is performed through direct cortical stimulation. With the invasive EEG electrodes that are places, brief electrical currents are delivered to the brain. This allows physicians to precisely identify the function of that specific brain area. Common functions that are mapped using cortical stimulation include speech, understanding, movement and sensation.
Is brain stimulation painful or dangerous?
Brain stimulation is typically not painful. Unusual sensations may be experienced for brief periods during the stimulation. There is also the potential to initiate a seizure during brain stimulation. This is why a neurologist is also present in order to read the EEG and be able to stop any seizure right away through medications.
Who performs brain mapping and how is this information incorporated into a surgical plan?
The brain mapping team consists of neuropsychologists, neurologists and neurophysiologists. The information gathered through this study is critical to the epilepsy surgery team to determine if surgery is feasible and safe. The team will be able to determine if the presumed onset of the epilepsy area is sufficiently away from the areas of the brain that control important functions. If this is a case, a surgical plan may be proposed with a high chance of seizure freedom with minimal to no expected side effects.