Sturge-Weber Syndrome
Find your care
Call 310-825-5111 to learn more about our world-class pediatric neurosurgery services.
Epilepsy Surgery for Sturge-Weber Syndrome
In this section: Tuberous Sclerosis Complex | Focal Cortical Dysplasia | Hemimegalencephaly | Rasmussen’s Encephalitis | Sturge-Weber Syndrome
Sturge-Weber Syndrome at UCLA
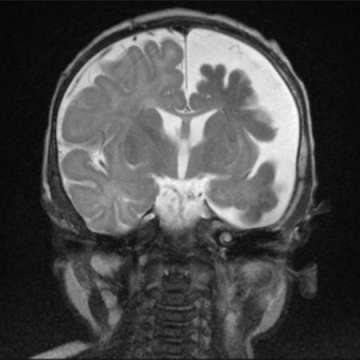
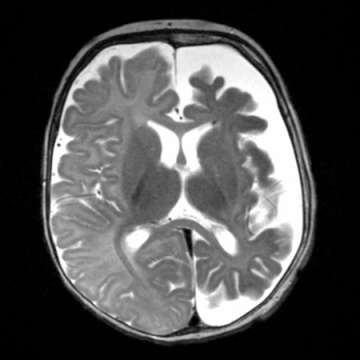
Sturge-Weber syndrome (SWS) is a rare vascular disorder present at birth that is characterized by facial blood vessel malformation (port wine stain) and associated blood vessel malformations affecting the brain and eye. It is not a heritable disorder. The “port-wine stain” on the face is typically isolated to one half of the face and commonly involves the upper portion of the face. This skin lesion is usually obvious at birth although its appearance can change with age as the child grows.
The cause of SWS is a somatic (i.e. non-inheritied) mosaic mutations in the GNAQ gene. The blood vessel malformations associated with SWS can lead to specific neurologic and ocular abnormalities.
Neurologically, the infant or child may present with seizures that are progressively more difficult to control with medications. In addition, neurological deficits and developmental delay may result. Visual field defects may also occur with variable severity. Hydrocephalus (i.e. too much brain fluid) also may occur. A small proportion of patients have no neurologic abnormalities.
The reasons for neurologic progression in SWS are uncertain. One possible mechanism is the lack of blood flow and oxygen to the surrounding brain.
Port wine stain — Cutaneous port wine stain (capillary malformation) is the most common type of vascular malformation, occurring in 0.3 percent of newborn infants (picture 1). However, only a small proportion of children with port wine stains have SWS. (See "Capillary malformations (port wine stains) and associated syndromes".)
In SWS, the port wine stain typically is present on the forehead and upper eyelid, primarily in the distribution of the first or second division of the trigeminal nerve
Although traditionally considered important in determining meningeal involvement risk, the location of the capillary malformation (port wine stain) on the face is not a good indicator of the risk of an underlying meningeal capillary malformation. However, the midface and the meninges do share a common embryological origin [4]. Extension of the skin lesion to both sides of the face and the trunk and extremities is common.
The skin lesion usually is obvious at birth. However, its appearance changes with age and its size increases as the patient grows. In the newborn, the lesion is flat and usually light pink in color. It typically darkens with age to a deep red, port wine appearance, and vascular ectasias develop (picture 2). The vascular ectasias produce nodularity and superficial blebbing, which lead to overgrowth of the underlying soft tissues and sometimes the bone. Dental abnormalities may occur as a result of gingival thickening if this area is affected. By the fifth decade, 65 percent of patients with a facial port wine stain have hypertrophy and nodularity within the lesion.