Positioning and Technique
by Connie Ju, MD, and Laura Doepke, MD
Introduction
Screening mammograms are performed in asymptomatic women and have been shown to reduce breast cancer mortality by more than 30% in women 40 and older through early detection of breast cancer.1 In order to achieve this end, adequate patient positioning and acquisition techniques must be utilized to promote visualization and high-accuracy interpretation.
The goal of mammography is to obtain quality imaging of the greatest amount of breast tissue possible, because breast cancer detection begins with good positioning. Compression paddles on the mammographic unit compress the breast tissue against image receptors. Although this may involve temporary discomfort, good compression is imperative for obtaining quality mammographic images by reducing overlapping tissue, immobilizing the breast to reduce motion artifact, and creating uniform thickness of the breast tissue.2
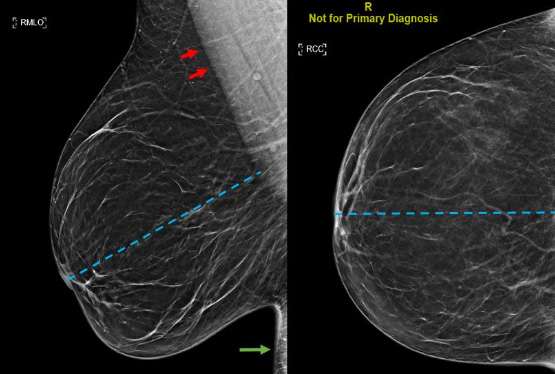
The standard mammographic views are the mediolateral oblique (MLO) and craniocaudal (CC) view. Obtaining at least two views of the breast allows for more breast tissue to be imaged and therefore offers a more comprehensive screening exam. Two views allows for better localization of underlying abnormalities that cannot be deciphered on a single view alone. It is important for the technologist to attempt to obtain views of the breast with the nipple in profile, ideally in both views, but in at least a single view to follow guidelines and to allow for adequate visualization of the breast tissue, particularly the subareolar region. The posterior nipple line (PNL), a line drawn at a 45 degree angle from the nipple towards the anterior aspect of the pectoralis on the mediolateral oblique view, is used to assess adequate imaging quality (Figure 1).4
Mediolateral Oblique (MLO) View
A good mediolateral oblique (MLO) view provides visualization of the greatest amount of breast tissue, including the posterior breast and axillary region (Figure 1). When obtaining an MLO image, the breast is placed on the image receptor which lies parallel to the pectoralis muscle. The compression paddle then compresses the breast from a superomedial direction. In order to determine whether acquisition technique is adequate, it is important to assess three factors: the presence and position of pectoralis muscle, the posterior nipple line (PNL), and the inframammary fold.3
Ideally the margins of the pectoralis muscle appear as straight lines or convex curves, which implies breast tissue has been sufficiently pulled forward. The posterior nipple line should be able to intersect the pectoralis muscle at a perpendicular angle. The inframammary fold (IMF) is the most inferior portion of the breast which intersects the chest wall and should be included in the MLO image. Inclusion of the IMF promotes detection of masses that may be located in this most inferior aspect of the breast.
Craniocaudal (CC) View
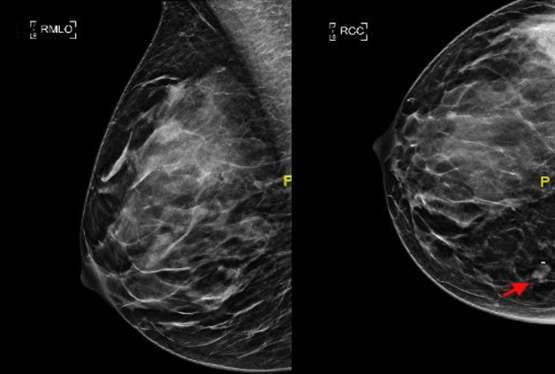
In the ideal craniocaudal view, the nipple should be positioned midline and the length of the PNL should be within 1 cm from that of the MLO view (Figure 1). The image receptor is positioned beneath the breast and compression is applied superiorly. When positioned correctly, the craniocaudal view has the advantage of showing the deep medial breast tissue which is often excluded on the mediolateral oblique view. Thus, it is imperative to ensure adequate inclusion of the deep medial breast in the CC view to detect masses that are otherwise excluded in MLO views (Figure 2).
Implant Displaced Views
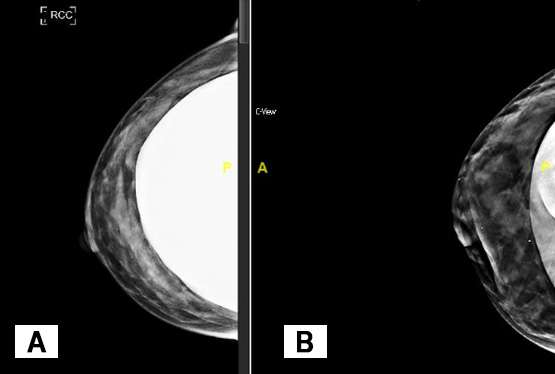
Breast implants appear dense on mammographic images and can obscure normal breast tissue. For patients with breast augmentation, the Mammographic Quality Standards Act recommends two additional views of each breast in addition to the standard views described in the aforementioned text.2 While the standard MLO and CC views are obtained with the implant included and with lighter compression to prevent implant rupture, the additional “implant displaced” views are performed under normal compression with as much of the implant excluded from the image as possible (Figure 3). A closer evaluation of normal breast parenchyma can be assessed on the implant displaced views while the implant included views allow for visualization of both the implant and a general overview of the breast.
References
- https://www.sbi-online.org/endtheconfusion/FactsFigures.aspx
- Ortiz-Perez T, Watson AB. “Mammography Techniques, Positioning, and Optimizing Image Quality.” Breast Cancer Screen Diagnosis A Synopsis. January 2015:37-63. doi: 10.1007/978-1-4939-1267-4_3
- Nguyen J V., Rochman CM, Nicholson BT. “Imaging the Screening Patient.” In: Brant and Helms’ Fundamentals of Diagnostic Radiology. 5th ed. Wolters Kluwer; 2019.
- Bassett LW, Doepke L: Clinical Image Evaluation. Chapter 7. Pages 121-132. Bassett LW, Mahoney MC, Apple SK, D’Orsi CJ (eds): Breast Imaging. Philadelphia: Elsevier, 2010