Breast MRI Indications
by Natalie Cain, MD, and Jane Dascalos, MD
Basic Principles
Breast magnetic resonance imaging (MRI) is an invaluable tool for breast imaging practice and interventional procedures when utilized in the appropriate clinical setting. It has the highest sensitivity for breast cancer detection, ranging from 75.2%-100% with a positive predictive value for biopsy comparable to mammography between 11%-40%1. Its high sensitivity is believed to be due to tumor neoangiogenesis, which results in the creation of leaky vessels associated with a breast cancer2. Gadolinium-based contrast agents are able to escape from these leaky vessels and accumulate within a malignancy, allowing for easy visualization on MRI. Thus, unlike mammography, breast MRI is not limited by dense breast tissue. Although benign conditions can also demonstrate enhancement, lesion morphology and enhancement kinetics help distinguish them from cancer.
Indications
Screening
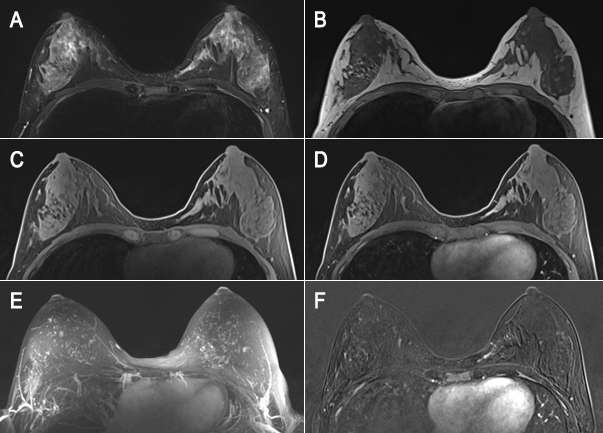
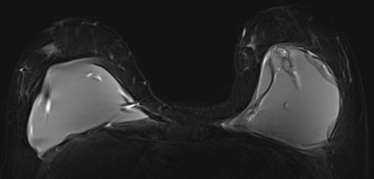
Breast MRI is indicated for annual breast cancer screening in women with a high risk of developing the disease. High-risk is defined as having a greater than or equal to 20% lifetime risk of breast cancer, which is based on certain criteria that put the patient at risk. Some of the criteria in determining high risk include genetic predisposition, family history and prolonged estrogen exposure. Women without an increased risk for breast cancer benefit less from MRI because the false-positive rate may significantly exceed the cancer detection rate, and further investigation of the findings can lead to additional workups and benign biopsies. However, screening MRI may be appropriate for average-risk women with a history of direct free silicone injections of the breast for augmentation due to the difficulty of mammography in these cases. Other indications in those with genetic predisposition include BRCA mutation carrier (including BRCA1 and 2), an untested patient with a first-degree relative with the BRCA mutation, Li Fraumeni syndrome (p53 mutation) and first-degree relatives, and Cowden and Bannayan-Riley-Ruvalcaba syndromes in first-degree relatives. Lastly, patients who underwent mantle radiation to the chest wall between the age of 10 and 30 years for Hodgkin lymphoma have been shown to benefit from screening MRI due to their increased risk of breast cancer. It is important to note that annual breast MRI screening should be supplemented by mammography and compared to all other available breast imaging modalities because MRI will miss some cancers that mammography can better detect.
Staging
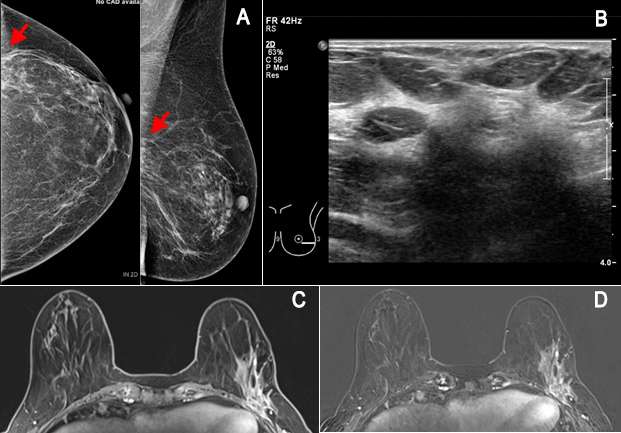
MRI is often used preoperatively to image the extent of breast cancer, including assessment of chest wall invasion, satellite lesions or multifocal/multicentric disease (additional cancer) to guide management and surgical approach. However, it is a somewhat controversial indication without additional high risk factors because the detection of more disease at MRI has not translated to improved outcomes or survival3. For instance, breast MRI is indicated in patients with biopsy-proven invasive lobular carcinoma due to its propensity to be multifocal/multicentric and affect the ipsilateral breast, which is seen in 20-29% of cases4. Studies have consistently shown a decreased repeat surgery rate when preoperative MRI was utilized3. Although somewhat controversial, breast MRI has been used in evaluating the extent of disease in patients with dense breasts where mammographic assessment was suboptimal. It can also be a useful tool to detect the primary breast cancer in patients with biopsy-proven axillary lymph node metastasis and normal mammogram and ultrasound5. Lastly, breast MRI has been shown to be successful in detection of residual disease after lumpectomy with positive margins, which is seen as asymmetric and nodular enhancement that is noncontiguous with the biopsy site5.
Management of Patients Undergoing Neoadjuvant Therapy
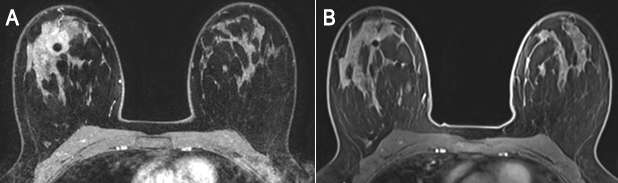
Breast MRI is indicated in patients undergoing neoadjuvant therapy (chemotherapy prior to surgery) to assess disease response. The tumor measurement is most accurate on MRI, as sonography and mammography typically underestimate tumor size. Therefore, breast MRI is the most accurate imaging modality to assess tumor response, with a positive predictive value of 93%6. Imaging the patient before treatment and after completion of one to two cycles can help predict how well the patient is responding to neoadjuvant therapy. In patients who do not respond, MRI after completion of the regimen can be performed to identify and localize residual tumor5.
Additional evaluation of clinical or imaging finding
There are few circumstances where MRI is used as an adjunct to diagnose equivocal (uncertain) findings on mammography, sonography or physical examination. The first indication is a patient with persistent bloody or cytologically abnormal nipple discharge. MRI may also be useful for a suspicious finding seen only on one mammographic view that is not amenable to conventional biopsy. Breast MRI is also indicated in the evaluation of clinically suspected silicone implant abnormality or rupture. Due to its high spatial resolution and the contrast between implants and soft tissues, it has the highest sensitivity and specificity for implant rupture among imaging modalities and can be used to assess associated complications involving the surrounding breast tissue, chest wall and axilla7. Lastly, it can be used to evaluate patients with unclear but persistent physical examination findings that are mammographically and sonographically occult5.
Conclusion
Breast MRI is an excellent primary and supplemental tool in breast imaging practice when utilized in appropriate clinical and diagnostic situations. MRI for screening leads to earlier cancer detection, especially in high-risk women. It is invaluable in the assessment of extent of disease, post-surgical residual disease, high risk screening, and response to neoadjuvant treatment amongst other indications.
References:
- Mann RM, Kuhl CK and Moy L. “Contrast-Enhanced MRI for breast cancer screening.” Journal of Magnetic Resonance Imaging 2019; 50(2): 377-390. DOI: 10.1002/jmri.26654
- Carmeliet P, Jain RK. “Angiogenesis in cancer and other diseases.” Nature 2000; 407: 249– 257. DOI: 10.1038/35025220
- Mann RM, Cho N and Moy L. “Breast MRI: State of the Art.” Radiology 2019. 292:3, 520-536. DOI: 10.1148/radiol.2019182947
- Su Min Ha, Eun Young Chae, Joo Hee Cha et al. “Breast MR Imaging before Surgery: Outcomes in Patients with Invasive Lobular Carcinoma by Using Propensity Score Matching.” Radiology 2018. 287:3, 771-777. DOI: 10.1148/radiol.2018171472
- Ikeda, DM. Breast Imaging: The Requisites 2nd Edition. El Sevier 2011. https://www.elsevier.com/books/breast-imaging-the-requisites/ikeda/978-0-323-05198-9
- Fowler AM, Mankoff DA and Joe BN. “Imaging Neoadjuvant Therapy Response in Breast Cancer.” Radiology 2017. 285:2, 358-375. DOI: 10.1148/radiol.2017170180
- Juanpere S, Perez E et al. ”Imaging of breast implants – A pictorial review.” Insights Imaging 2011. 2:6, 653-670. DOI: 10.1007/s13244-011-0122-3