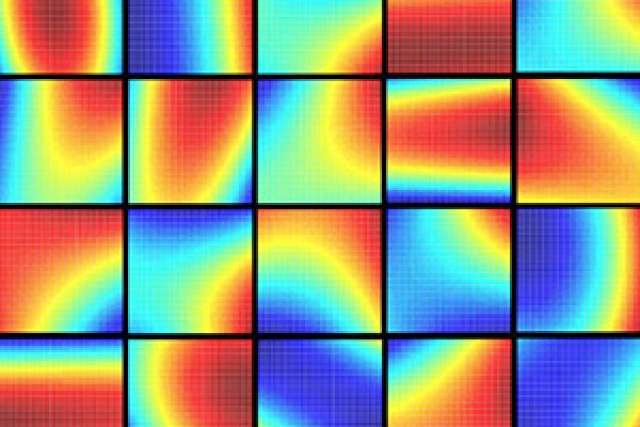
UCLA scientists say the finding that every patient’s response to medical treatment produces a parabola-shaped graph, like those here, is a landmark advance.
For decades, doctors and scientists have predicted that personalized medicine — tailoring drug doses and combinations to people’s specific diseases and body chemistry — would be the future of health care.
A team of UCLA bioengineers and surgeons has taken a major step toward that reality.
The researchers, from the UCLA schools of dentistry, engineering and medicine, developed a revolutionary technology platform called phenotypic personalized medicine, or PPM, which can accurately identify a person’s optimal drug and dose combinations throughout an entire course of treatment. Their research will appear online in the April 6 issue of the peer-reviewed journal Science Translational Medicine, a publication of the American Association for the Advancement of Science.
Unlike other approaches to personalized medicine currently being tested, PPM doesn’t require complex, time-consuming analysis of a patient’s genetic information or of the disease’s cellular makeup. Instead, it produces a personalized drug regimen based on information about a person’s phenotype — biological traits that could include anything from blood pressure to the size of a tumor or the health of a specific organ.
Dean Ho, who holds appointments in oral biology and medicine at the UCLA School of Dentistry, and in bioengineering at the UCLA Henry Samueli School of Engineering and Applied Science, said one of the platform’s remarkable capabilities is its ability to produce graphs personalized for each individual patient that represent precisely how they respond to treatment.
The graphs plot the drug dose along the horizontal axis and the patient’s response to treatment on the vertical axis. (Data for the patient’s response is dictated by whatever health goal the doctor is trying to achieve: shrinking the size of a tumor, having a certain level of medication in the blood or reducing toxicity level, for example.)
Remarkably, Ho said, every person produces a graph in the shape of a curve called a parabola — picture a “U” either right-side up or upside down — and that parabola dictates how doctors should proceed with the treatment. Each person’s unique curve provides doctors with a visual guide to determine the exact doses of medicine they should prescribe as the treatment continues, which Ho said is the key to achieving truly personalized medicine.
“This study demonstrated the ability to use a patient’s phenotype to personalize their treatment in an actionable manner without the need for genome profiling,” said Ho, a corresponding author of the study. “We also have shown that PPM can be extended to optimize combination therapy for a wide spectrum of diseases.”
Showing that every patient’s response to medical treatment — for diseases ranging from cancer to infectious diseases, or following an organ transplant — produces a parabola-shaped graph is a landmark advance, Ho said. Among other things, the approach will allow doctors to prescribe the precise amount of medicine needed to shrink a tumor or ensure the body doesn’t reject an organ, for example, as opposed to using a higher, “standard” dose that’s recommended based on an average of how all patients have responded in the past.
Another benefit of PPM is that it can be recalibrated in real time to adapt to changes during treatment — for example if a person undergoes surgery or develops an infection, or if their organ function changes over time, any of which could mean that drug dosages or combinations need to be modified. The platform can use the patient’s new data to provide doctors with a new parabola and revised recommendations.
Tested for post-transplant care
The new study evaluated eight people who had recently received liver transplants.
Most transplant patients take an immunosuppressive drug called tacrolimus to prevent their bodies from rejecting the organ. In general, doctors prescribe dosages of the drug based on how other patients have responded in the past, and they adjust those amounts if and when complications arise. In the UCLA research, four patients received care followed the traditional approach and four received treatment that was guided by PPM.
“Properly managing patients’ immunosuppression can have profound long-term impacts on the survival of the organ and the patient,” said Dr. Ali Zarrinpar, assistant professor of surgery in the UCLA division of liver and pancreas transplantation and a corresponding author of the study. “This study shows that we can pinpoint drug doses that can substantially improve patient outcomes. The ability to confidently and systematically guide the treatment of each patient is a critical advance in minimizing the chance that transplant recipients will reject their new organs, while also avoiding drug side effects.”
To know whether the PPM approach was successful, researchers wanted to see the amount of tacrolimus in each patient’s body stay within the “ideal” range, as dictated by each patient’s unique parabola-shaped graph. They found that those who were treated following PPM spent as much as 50 percent less time outside of that range than the patients whose treatment followed the traditional approach.
“Optimizing the drug ratios during combination therapy for a population or a specific patient has, until now, been virtually impossible,” said Chih-Ming Ho, who is UCLA Engineering’s Ben Rich–Lockheed Martin Professor, and a corresponding author of the study. “Our ability to calibrate how individual patients respond to treatment and to use that information to robustly guide their regimen based on the parabola-based approach has made personalized medicine a reality.”
Chih-Ming Ho, who holds faculty appointments in mechanical and aerospace engineering, and in bioengineering, pioneered the development of PPM.
The team is using PPM in several other clinical trials, some of which are already underway, including for treating cancer and infectious diseases.
Other authors of the study, all from UCLA, were postdoctoral researchers Dong-Keun Lee, Aleidy Silva and Sean Wang; graduate student Theodore Kee; Dr. Ronald Busuttil, the Dr. William P. Longmire Jr. Chair in Surgery and executive chairman of the department of surgery; Dr. Nakul Datta; Dr. Calvin Eriksen; Dr. Keri Weigle; Dr. Vatche Agopian; Dr. Fady Kaldas; and Dr. Douglas Farmer. Dean Ho, Chih-Ming Ho, Zarrinpar, Busuttil and Agopian are members of the UCLA Jonsson Comprehensive Cancer Center.
Support for the project was provided in part by the National Cancer Institute, the National Institutes of Health, the National Science Foundation, the V Foundation for Cancer Research, the Wallace H. Coulter Foundation, the Society for Laboratory Automation and Screening, Beckman Coulter Life Sciences, and the Endowment Fund of the Ben Rich–Lockheed Martin Chair Professorship.