As one of the pillars of cancer treatment, radiation therapy is often only seen as a treatment for this disease. While its primary use is, indeed, in treating various malignancies, its applications often expand beyond oncology.
Currently, Ann Raldow, MD, MPH, associate professor of radiation oncology at the David Geffen School of Medicine at UCLA and member of the UCLA Health Jonsson Comprehensive Cancer Center, is collaborating in a pioneering effort to eliminate the need for anti-rejection medication for organ-transplant patients through total lymphoid irradiation — priming the recipient's immune system to accept donor stem cells. This innovative approach has shown great promise in improving patients' lives.
In this interview, Dr. Raldow discusses what interested her about the field and the role of radiation therapy in oncology and beyond.
What inspired you to go into the oncology field?
I have been drawn to oncology since college when I shadowed a surgical oncologist. And while I loved that surgical oncologist’s clinic, I did not enjoy the actual surgical part as much. But I just loved his interaction with patients and how meaningful his work was to them. It’s a really tough time for patients and their families, and because of that, I think being there with them, and through the process, is that much more meaningful. I don't know if I can necessarily articulate it perfectly, but I just feel like it's a privilege to be there for someone when they're at their most vulnerable.
Why specifically radiation oncology?
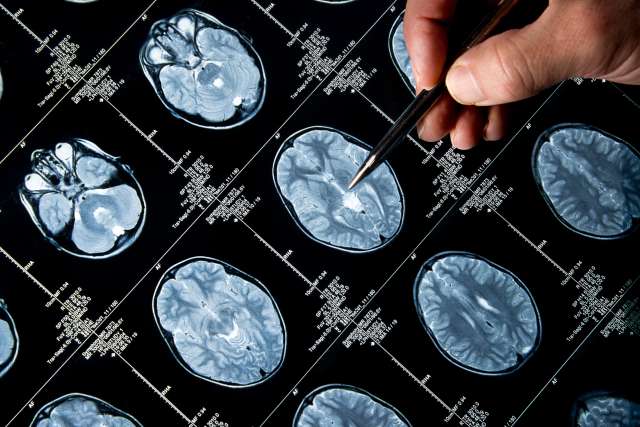
Radiation oncology is an absolutely amazing and meaningful field. I have always been interested in technology and how we can use technology not just for entertainment, but also for good, so that really drew me to radiation oncology. I love the toys that we have in this field, like MRI-guided radiation, as well as advanced treatment planning systems that result in conformal treatment plans using intensity-modulated radiation therapy (IMRT) and stereotactic body radiation therapy (SBRT). I like the technical aspects of it and how we're always trying to improve upon targeting the tumor while at the same time sparing as much of the normal healthy tissue as possible. I also love the bread and butter of what we do as radiation oncologists, which is contouring or delineating treatment targets on imaging. It's like coloring for adults. Basically, you get to draw on CT scans or MRI scans, which I think is very therapeutic and fun.
What is a typical day like for you?
Our schedule on a weekly basis is very different depending on what day it is. For instance, on Mondays I see patients who are currently on treatment. On Tuesdays, I have some academic time. I attend tumor boards, I have some clinical research meetings or clinical trial meetings, and then I see new patients in the afternoon. I tend to follow up with new patients on Wednesdays and then Thursday is purely academic, where I do research and meet with folks. And then I split Fridays. The morning is dedicated to academics and then I have a clinic in the afternoon. In those academic times, there's also quite a bit of time that we dedicate to treatment planning so I feel like every day is different in terms of what I do.
You mention you have specific time dedicated to research. What does your research focus on?
I do both clinical research and health services research. My two major focuses are on quality of life and cost effectiveness. I think it's very meaningful work if you can make a tangible difference in how patients go through treatment. One of the things I've been working on is technology that helps patients self-report symptoms. This can help patients feel more engaged in their treatment journey. And we as clinicians are able to act quicker on their symptoms.
Radiation is a big part of cancer treatment. How is radiation therapy used for other types of issues, like transplants?
Radiation, of course, is mostly used to treat cancer. There are some benign indications for radiation such as the prevention of heterotopic ossification for patients who are in motor vehicle accidents and other traumas that get orthopedic surgery.
Radiation, or total lymphoid irradiation, is also part of the kidney transplant protocol under the leadership of Dr. Jeffrey Veale here at UCLA to eliminate the need for anti-rejection medication. Creating tolerance in an organ recipient requires radiation treatment to help prime the recipient’s immune system to accept the donor’s stem cells.
So far, it's been quite successful. Patients have been able to achieve chimerism, so they have been able to ultimately recognize the donor kidney as self, in addition to their own tissue as self. Achieving chimerism prevents the body's usual reaction to try to reject the organ and avoids the need for immunosuppressive drugs for patients going forward. And that's huge because nobody wants to take immunosuppressive drugs for the rest of their life. Not only is it a pain, but there's a lot of side effects or negative consequences of having to take the immunosuppressive drugs. Patients are more immunocompromised and more susceptible to developing malignancies in the future.
My role for this particular study is to design and administer the total lymphoid irradiation for patients. The radiation has to be very carefully timed with the rest of the treatment that the patient is undergoing. And of course, while the patient is having the radiation treatments, I see them for weekly treatment visits just to check in see how the patient's doing and deal with any side effects that come up. As of now, patients undergoing the radiation are tolerating it really well with minimal side effects, which is great.
Take the Next Step
Learn more about Radiation Oncology services at UCLA Health.