What is a Mastectomy?
Find your care
UCLA Health’s Breast care specialists develop a personalized plan to help you recover. For more information, reach a cancer care specialist at 310-825-2144.
Mastectomy
Although a mastectomy involves removal of as much of the underlying breast tissue as technically possible, there are variations in how much of the overlying skin envelope is preserved. The sensation to the skin that is left behind, however, is forever altered and generally numb. This occurs because the sensory nerves that innervate the skin are divided when the breast tissue is dissected off of the undersurface of the skin.
Total (simple) mastectomy: In this procedure, all the underlying breast tissue is removed, as well as the excess overlying skin and the nipple and areolar complex.
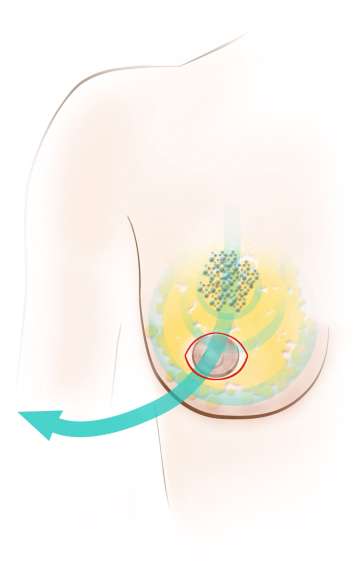
Skin-sparing mastectomy
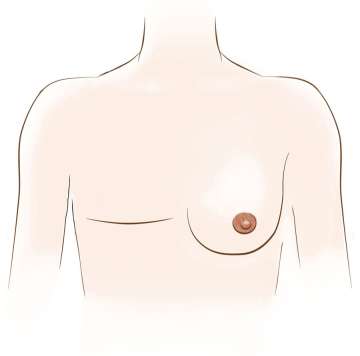
In this procedure, all the underlying breast tissue is removed as well as the nipple and areolar complex with sparing of as much of the overlying native breast skin as possible. This can be accomplished through an incision around the areola or a small elliptical incision including the nipple and areola (see illustration). This specialized approach helps the patient undergoing immediate breast reconstruction preserve the natural shape and contour of the breast by keeping the outer envelope of skin intact. Multiple published series have shown that using a skin-sparing approach in cases where immediate breast reconstruction is planned leads to high rates of patient satisfaction without increased risk of recurrence.
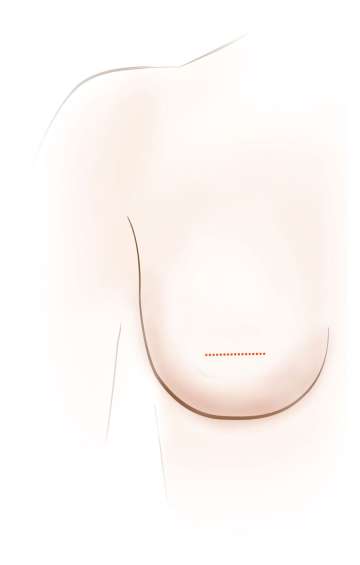
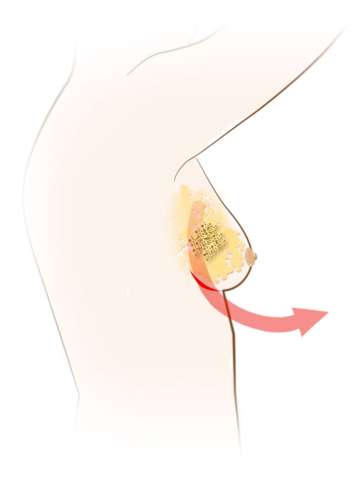
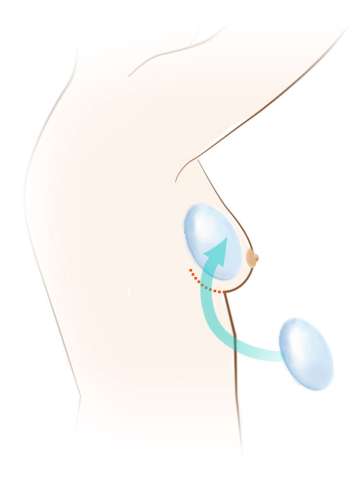
Nipple-sparing mastectomy
A highly specialized form of a simple mastectomy, a nipple-sparing mastectomy involves removal of all the underlying breast tissue while preserving the entire outer envelope of skin with the nipple and areola intact. Because breast ducts traverse through the nipple and allow a woman to breast feed, the nipple ducts must be clear of any cancerous cells on pathology checked during surgery in order to safely leave the nipple behind. There are many different incisions used to do this surgery. One incision is made under the fold of the breast. Other incisions begin near the areola and extend towards the outer portion of the breast. Two large studies have shown that a nipple-sparing approach is safe in carefully selected patients. If you are planning to have a mastectomy and immediate reconstruction, ask your surgeon to see if you are a candidate for this approach.
Modified radical mastectomy
This operation involves removing the entire breast as well as two levels of lymph nodes under the armpit (see Lymph Node Surgery). No muscle is removed from the chest wall under the breast.
Multiple factors such as type of cancer, location of cancer, natural breast shape and size, and cosmetic goals are considered when determining which type of mastectomy and/or reconstruction is best for you. Your breast surgeon will help you understand your options and guide you towards making the best choice for you.
Shouldn’t I Just Choose Mastectomy if I Want the Best Chance of Cure?
If a mastectomy was the better surgery and resulted in greater overall survival for patients, a lumpectomy would not be offered as a suitable alternative to mastectomy for patients with breast cancer. However, the best data show that the cure rates for lumpectomy for treatment of early stage breast cancer are equivalent to that for mastectomy. Well, why might that be?
The goal of breast cancer treatment is two-fold: 1) to treat the cancer in the breast and prevent it from coming back in the breast, and 2) to treat the microscopic cancer cells that may be in the blood and prevent those cells from seeding another organ and becoming metastatic disease. For some breast cancers, local treatment may be enough but for many cancers, treatment of the circulating tumor cells in the blood is essential for cure. Surgery and radiation can only treat the cancer cells that are within its reach. Tumor cells in the blood are out of the reach of surgery and radiation, and are treated by medical therapies, like the hormone blocking pill and chemotherapy. Because it is treatment of the tumor cells in the blood that determines cure, which surgery is performed to remove the cancer in the breast does not impact the cure rates and overall survival.
What surgery does impact is local recurrence rates, or the risk of the cancer returning in the breast, not other organs. With radiation, the risk of the cancer coming back in the breast after a lumpectomy is generally < 5-10%. Following a mastectomy, radiation is often not needed and the risk of the cancer returning can be as low as 1- 2%. The overall risk of a new separate breast cancer occurring in the same breast after lumpectomy because the rest of the breast was left in place is approximately 2%. A patient with a diagnosis of breast cancer who is treated with breast conservation surgery has about a 0.5% per year risk that she will develop a breast cancer in the opposite breast sometime during her lifetime that is unrelated to her original cancer. It is important for patients to realize that most women do not have a high risk of getting a cancer in the opposite breast after breast conserving surgery, so removal of a healthy breast not affected by breast cancer is generally not recommended.
Treatments exist for every type and stage of breast cancer. Talk with your doctor to learn as much as possible about your surgical treatment options. Just as no two women are the same, no two breast cancers are the same, and it is important to try to understand the best choice for you.
Phone: 800-UCLA-MD1 or 424-424-0273