Breast Cancer – Brachytherapy
Find your care
Radiation oncologists use a patient-centered approach and individualized treatment plans. To learn more and make an appointment with a UCLA radiation oncologist, contact us at:
Westwood - 310-825-9775
Santa Clarita - 661-287-0010
Santa Monica - 424-259-8777
El Segundo - 310-794-7301
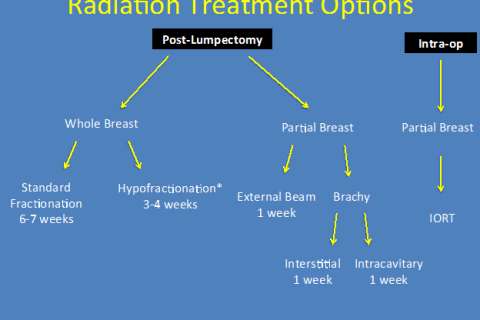
What are my Options for Radiation?
Here, at the UCLA Radiation Oncology Division of Brachytherapy, we are committed to making your cancer treatment a comfortable and successful experience. With over 30 years of experience, we have some of the most expertise on the use of HDR Brachytherapy for breast cancer in the nation.
At UCLA, we have the resources to deliver radiation therapy in the operating room.
In our clinic, Intra-Operative Radiation Therapy (IORT) is being used to treat breast cancer. It is a newer form of partial breast radiation which is done from start to finish in the operating room in conjunction with the surgery. IORT for breast is a type of breast brachytherapy or APBI (Partial Breast Irradiation). It is designed to reduce radiation exposure to just those areas at most risk for recurrence and it maximally limits treatment to the normal surrounding tissue. In the case of IORT breast, the radiation is given in the operating room when the tumor bed is exposed. In many cases, no additional radiation therapy is needed. IORT is typically used for smaller and more favorable breast cancers. We also employ other brachytherapy methods and the latest external beam techniques for breast cancer to best fit the individual patient needs.
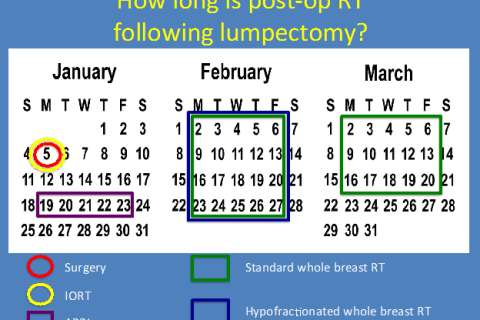
How long will I be receiving radiation treatment for?
The length of time you will receive radiation will depend on the type of treatment that is most appropriate for you. It can be as long as 6-7 weeks and possibly as short as 1 treatment. The calendar below demonstrates the various lengths of time of the different treatments:
What is APBI
Accelerated partial breast irradiation (APBI) refers to radiation treatment that is focused to just the cavity where a lumpectomy was performed as opposed to the whole breast.
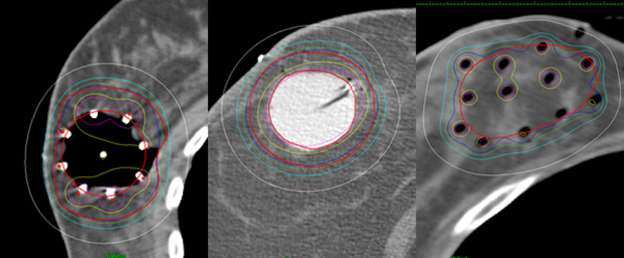
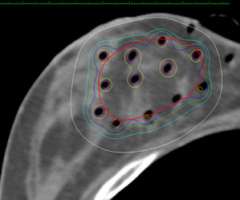
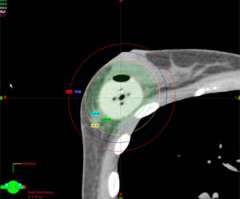
Examples show how the radiation dose (the colored lines, with the white lines representing 50% of the dose) is targeted to the area where the original tumor was using three different partial breast radiation techniques (SAVI, Contura, Tube and Button).
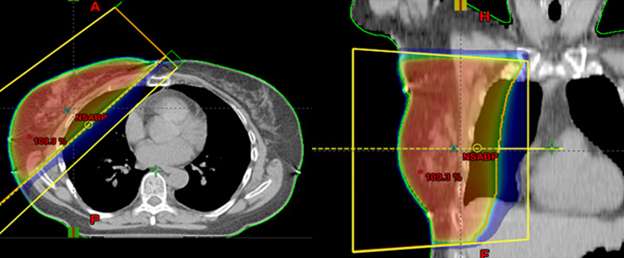
This is in contrast to these examples of standard whole breast radiation where the entire breast is considered the target.
Choosing APBI as a Treatment
The rationale for APBI is that the majority of recurrences in the breast occur around the site of the original lumpectomy cavity. By limiting the radiation to just the area around the lumpectomy cavity the treatment can be completed in a shorter period of time and exposes less normal tissues like the skin, heart, and lungs to unnecessary radiation exposure.
Who is a candidate for APBI?
Decisions regarding who is an appropriate candidate for APBI are ultimately made by the treating physician and the patient after a formal consultation and review of the patient’s history, imaging, and pathology. However, in general, candidates for APBI include:
- Age ≥ 50
- Invasive ductal carcinoma or Ductal Carcinoma In Situ disease
- Lesions ≤ 3 cm
- Negative surgical margins
- Negative Sentinel Lymph Node
- No pre-operative chemotherapy
Results of APBI
There are multiple studies demonstrating the safety and efficacy of APBI. The most important study, to date, on APBI was however published in 2015.
In 2015 the results of a phase 3 randomized trial of APBI versus whole breast radiation was published. Over 1,000 women were enrolled on this trial between 2004-2009 and at 5-year follow-up the cumulative incidence of local recurrence was not significantly different at 1.4% with APBI and 0.92% with whole breast radiation. There were also no significant differences in serious long term side effects between the two treatments. This is the most important study published to date on APBI and provides Level 1 evidence regarding the use of APBI in appropriately selected women.
Reference:
Lancet. 2015 Oct 19. pii: S0140-6736(15)00471-7. doi: 10.1016/S0140-6736(15)00471-7.
5-year results of accelerated partial breast irradiation using sole interstitial multicatheter brachytherapy versus whole-breast irradiation with boost after breast-conserving surgery for low-risk invasive and in-situ carcinoma of the female breast: a randomised, phase 3, non-inferiority trial.
StrnadV1, Ott OJ2, Hildebrandt G3, Kauer-Dorner D4, Knauerhase H5, Major T6, Lyczek J7, Guinot JL8, Dunst J9, Miguelez CG10, Slampa P11, Allgäuer M12, Lössl K13, Polat B14, Kovács G15, Fischedick AR16, Wendt TG17, Fietkau R18, Hindemith M19, Resch A4, Kulik A20, Arribas L8, Niehoff P21, Guedea F10, Schlamann A19, Pötter R4, Gall C22, Malzer M22, Uter W22, Polgár C6, Groupe Européen de Curiethérapie of European Society for Radiotherapy and Oncology (GEC-ESTRO).
Types of APBI and description of insertion techniques
There are three types of APBI brachytherapy:
Interstitial tube and button
This technique is the original way that breast brachytherapy was done and the technique for which we have the longest follow-up. It is extremely versatile in terms of its ability to conform the dose to the target and minimize dose to normal tissues. One of the reasons that it has become less popular is that it’s a highly skilled procedure and not enough radiation oncologists have adequate training to do it. Here at UCLA we have extensive experience in breast interstitial tube and button and are able to offer it as an option when appropriate.
Description of the Technique
This procedure is performed in the outpatient surgery center or our brachytheraoy suite. It typically takes about 1-2 hours. At the end of the case a series of hollow little tubes will have been placed that encompasses the area where the tumor was.
After the procedure the patient will be brought to the Radiation Oncology Department for a CT simulation. This is a CT scan that allows us to verify the proper position of the hollow tubes and is used for treatment planning. Patients go home the same day and return to the department to start treatment the next day.
Single-entry applicators (SAVI, Mammosite, and Contura)
Interstitial tube and button requires a high skill set that not many physicians have so attempts were made to make breast brachytherapy “easier”. This led to the development of single-entry applicators. The single-entry refers to the fact that there is a single small incision (~1-2 cm) that is made in the breast where the applicator fits through (typically a site separate from the lumpectomy surgery incision). The three most common single-entry applicators are SAVI, Mammosite, and Contura. These applicators are either strut based (SAVI) or balloon based (Mammosite, Contura). The applicator that is used is based on multiple factors including the cavity size, proximity to the skin and chest wall, and the shape of the cavity.
The first single-entry applicator that was developed was the Mammosite single channel applicator that was FDA approved in 2002. The single channel refers to the fact that there is only one channel for the radiation source to travel through. As the radiation emanates out equally in all directions this means that the radiation dose is distributed essentially in concentric circles and can’t easily be pulled away from normal tissues. While this is not a problem for targets located in the center of the breast that are not close to the skin and/or the chest wall it is an issue for targets that are closer to important normal tissues. So in essence only women with cavities not too close to the skin or too close to the chest wall used to be appropriate candidates for partial breast treatment.
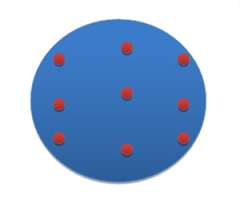
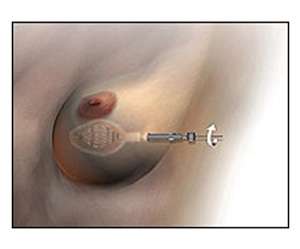
A cartoon depiction of the tube and button implant showing the entrance and exit sites of the hollow tubes.
Evolution to Multichannel Applicators
To improve our ability to “bend” radiation away from close targets like the skin and chest wall multichannel applicators were developed to provide more flexibility. This advance has dramatically increased the number of women eligible for partial breast treatment because of our improved ability to control the dose of radiation to the skin and the chest wall.
There are 3 multichannel applicators:
SAVI (we are a SAVI center of excellence)
To be a SAVI center of excellence a facility’s physicians, medical physicist and clinical staff are required to complete a comprehensive training and education program in order to demonstrate proficiency in delivering radiation therapy with SAVI.
Mammosite Multichannel Applicator
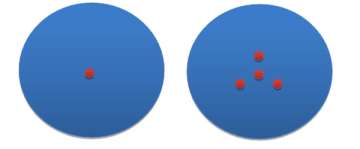
Each of these applicators is designed differently. The MammoSite and Contura are both balloon based applicators meaning that the channels that the radiation source travels through are located inside a balloon that gets filled with saline to conform to the shape of the lumpectomy cavity. The positioning/arrangement of the channels for the MammoSite and Contura are also more centralized as can been seen in the cartoon depictions above. The SAVI device is not balloon based but is strut based. These struts go in collapsed and then a turn-key is used to open up and expand the struts so that they sit on the edges of the lumpectomy cavity.
There are pros and cons to each applicator. We have extensive experience in doing partial breast treatment with all 3 of these applicators and base our applicator selection on multiple factors including breast size, cavity size, and proximity of the cavity to the chest wall and skin.
Description of the Applicator Insertion Technique
About 1-2 weeks following a woman’s lumpectomy surgery she will be seen in the Department of Radiation Oncology by one of our breast cancer specialists. At this time we will review the final pathology and to determine if the patient is a candidate for partial breast radiation. If she is then we use ultrasound and/or a CT scan to evaluate the lumpectomy cavity. What we are looking for on ultrasound or CT is whether there is a seroma (a cavity that is filled with fluid which normally forms following surgery where the breast tissue was removed). Our evaluation includes whether there is a seroma, how big it is, and its relationship to the skin and the chest wall. If a patient does not have a seroma, it is too small, or it is located too close to the skin and/or chest wall than a single-entry applicator may not be ideal and the interstitial tube and button approach may be recommended.
The actual placement of single-entry applicators is a simple office based procedure and is ideally done 2-4 weeks after surgery. The insertion technique is similar for all three applicators (MammoSite, Contura, and SAVI). Here at UCLA a radiation oncologist who specializes in brachytherapy will place the applicator. This is unique as these applicators are more typically placed by breast surgeons. Our radiation oncologists have special training in placing these applicators and are very experienced in it. Having the radiation oncologist place the applicator facilitates the process for the patient because all of the subsequent steps following applicator placement, such as CT simulation, can happen more quickly and smoothly as the patient does not need to travel from her breast surgeon’s office to radiation oncology. It allows us to understand the anatomy, any issues with the applicator, treatment planning, and be more insightful about the overall management of the patient.
The applicator is placed in our brachytherapy suite which is located in the Department of Radiation Oncology. This is a new state of the art facility designed just for brachytherapy patients. The procedure takes about 1 hour. Some women prefer to take a small dose of Ativan prior to the procedure but this is not mandatory. Otherwise only a small amount of local anesthetic is used. The area where the applicator will be inserted through will be cleaned and draped. An ultrasound will be used to evaluate the breast cavity. Some lidocaine will be used to numb the breast and the tract along which the applicator will be placed. Following this a small 1-1.5 cm incision will be made and a tract will be made for the applicator. The applicator will then be inserted through this track and visualized under ultrasound guidance. After the applicator is appropriately positioned in the lumpectomy cavity the device will be expanded until it fits sung against the cavity. Following placement of the applicator, a CT scan will be performed to allow us to verify the positioning of the applicator and also used for treatment planning. Dressings will be applied on the breast before patients are discharged home. This procedure is very well tolerated.
Patients can then go home and return to clinic to start their treatment the next day. After the patient goes home the images from the CT simulation are sent to our treatment planning computers and our medical dosimetrist and physicist work on a plan that will optimize coverage to the target and minimize dose to normal tissues.
When you go home after the applicator is placed there will be a small soft and flexible portion of the applicator that sticks out from the skin. This is gently held in place against the skin with gauze dressings and an ace-wrap. The dressing and applicator will not be noticeable underneath your clothes. We anticipate that women will be able to go about their normal everyday activities while the applicator is in place. The area should be kept dry so women should not take regular showers while the applicator is in place. We also recommend not doing any vigorous exercises to minimize the chances that the applicator is displaced.
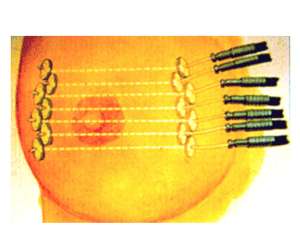
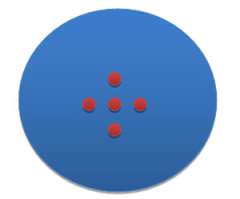
This is a cartoon example of a SAVI applicator sitting inside of a lumpectomy cavity and showing that a turn-key is used to expand the struts of the applicator so that it fits snug along the edges of the cavity.
Intra-operative radiation therapy (IORT)

Intraoperative treatment is another way partial breast treatment can be delivered. Here at UCLA we have a clinical trial open to offer this treatment using the Xoft machine.
This machine can be brought into the operating room at the time of lumpectomy and a balloon like device can be placed inside of the lumpectomy cavity.
This device is then connected to the Xoft machine to deliver a single dose of radiation over about 10-20 minutes. The concept is that a woman would wake up from surgery and potentially be done with her lumpectomy and radiation therapy.
There are some limitations to this technique which include not knowing the final pathology from the surgery until after the treatment has been given. Depending on the final pathology results a woman may or may not need additional radiation.
Description of actual daily treatments
When you start treatment they will be given 2 times per day for a total of 10 treatments. One treatment is given in the morning and the other is given in the afternoon. The treatments take about 10 minutes. Prior to each treatment some form of imaging is performed to verify that the applicator hasn’t changed position. If it has, then minor adjustments are made prior to starting treatment. This pre-treatment imaging and the actual treatments are done by a radiation therapist. Prior to starting treatment the applicator will be connected to the afterloader by a set of transfer tubes. The actual treatment is delivered in a brachytherapy treatment vault. There is a camera and microphone in the room should you need to communicate anything to us during the treatment. During the treatment you will hear the motor pushing the cable with the source on the end of it but otherwise you won’t feel anything or see anything. Some patients read during treatment, others listen to music, and some just fall asleep.
The daily treatment process is similar for interstitial tube and button and single entry applicators.
Women with Breast Augmentation
45-65% of women with breast augmentation following whole breast radiation develop capsular contraction. This can impact the cosmetic outcome of the implant and possibly require surgical revision. Outcomes for 110 women with breast augmentation treated partial breast radiation between 2003 to 2010 was presented at the 2011 American Brachytherapy Society meeting. With a median follow-up of 33 months there were no instances of implant failure or capsular contraction. 1 patient developed a same breast recurrence.
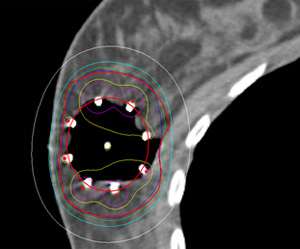
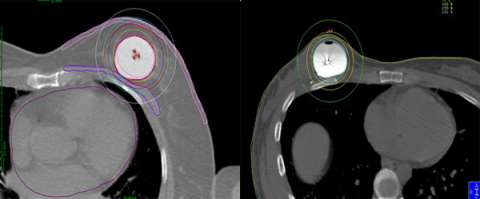
Below is an example of a case here at UCLA where we were able to spare the majority of the implant from receiving unnecessary radiation while achieving optimal coverage around the lumpectomy cavity.
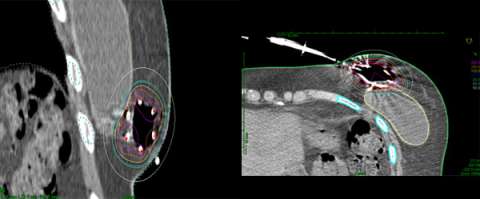
Example of a partial breast case done at UCLA in a woman with breast augmentation who had a SAVI applicator placed. One can see that the distribution of the radiation dose as can be seen in the colored lines is focused around the lumpectomy cavity and that the majority of the implant (light grey) is spared from unnecessary radiation. A different view of the same patient with the SAVI applicator in the lumpectomy cavity just above the implant outlines in yellow.
Side Effects of APBI
In the short term women may develop some skin redness around the area of treatment. This usually occurs about 1-2 weeks following the completion of treatment. There is a low risk of pain or infection while the applicator is in place. In the long term (month-years) after the treatment has been completed there is a high chance of good/excellent cosmesis and a low risk of any significant side effects including: persistent seroma, fat necrosis, or chest wall pain.
Follow-Up Care After APBI
The follow-up care after APBI is identical to that following whole breast radiation. Patients will be seen in follow-up every 6 months for the first 5 years and will have yearly mammograms performed.
Patient Resources and Support
Resources for Cancer Patients
Support Groups
Dealing with a diagnosis of breast cancer is life altering and challenging on many levels. Here at UCLA there are many resources to help patients, family, and friends manage the changes in their lives. We highly recommend patients to spend some time looking through the website of the Simms Mann Integrative Oncology center (http://www.simmsmanncenter.ucla.edu/) here at UCLA which provides free services for our cancer patients.
UCLA Publications on APBI
Kamrava M, Kuske RR, Anderson B, Chen P, Hayes J, Quiet C, Wang PC, Veruttipong D, Snyder M, Jeffrey Demanes D.
Ann Surg Oncol. 2015 Dec;22 Suppl 3:404-11. doi: 10.1245/s10434-015-4563-7. Epub 2015 Apr 28.
Brachytherapy catheter spacing and stabilization technique.
Demanes DJ, Friedman JM, Park SJ, Steinberg ML, Hayes JK Jr, Kamrava M.
Brachytherapy. 2012 Sep-Oct;11(5):392-7. doi: 10.1016/j.brachy.2012.01.010. Epub 2012 Mar 19.
The efficacy of breast MRI in predicting breast conservation therapy.
Blair S, McElroy M, Middleton MS, Comstock C, Wolfson T, Kamrava M, Wallace A, Mortimer J.
J Surg Oncol. 2006 Sep 1;94(3):220-5.