Our Stories

Priyam V. Tripathi, MD, joins Angie Jones at UCLA Health-Chargers cancer awareness game
On October 5, UCLA Health partnered with the Los Angeles Chargers to host a Crucial Catch game at SoFi Stadium, raising awareness for cancer prevention and early detection. Angie Jones, a participant in the 2023 UCLA Health Colorectal Awareness Campaign, was honored at the event for taking proactive steps to get screened for colorectal cancer. When Angie learned she was due for her first colonoscopy, Dr. Priyam V. Tripathi, health sciences assistant clinical professor of medicine, performed the procedure and discovered a large pre-cancerous polyp. The polyp was promptly removed, and ongoing monitoring has shown no evidence of disease. Grateful for the early detection and care she received, Angie invited Dr. Tripathi to join her and her family at the game to celebrate the impact of preventive care.

A colonoscopy may have saved this patient’s life, even though he put it off for six years
Val Gueorguiev had his first colorectal cancer screen in 2016 when he was 58. At the time, he chose to have a sigmoidoscopy because it seemed safer and easier, he said, and doesn’t require sedation. During the procedure, Dr. Kevin Ghassemi, UCLA Health gastroenterologist, removed a polyp, but also recommended that Gueorguiev have a colonoscopy as soon as possible. It wasn’t until six year later that Gueorguiev took his advice. Gueorguiev was impressed with the amount of time Dr. Ghassemi spent explaining the differences in the procedures and the importance of having a colonoscopy. Today, Gueorguiev is extremely grateful to Dr. Ghassemi, who was able to remove a pre-cancerous polyp that would have been missed with a sigmoidoscopy. Gueorguiev even convinced his wife and several friends to undergo colonoscopy. Read full story on the Jonsson Comprehensive Cancer Center blog

Competitive athlete Hilary Witbrodt's greatest victory? Her win over colorectal cancer
On paper, there was nothing about Hilary that put her in a higher risk category for colorectal cancer. She was incredibly fit – an endurance sports enthusiast who regularly competed in adventure racing: a combination of mountain biking, outrigger paddling and distance running. Her diet was high in whole grains and fruits and vegetables and low in processed foods. And she had no family history of colorectal cancer or related polyps, nor any personal history such as prior inflammatory bowel disease. Plus, she was only 41 – still several years away from starting regular preventive screenings. But in November of 2022, Witbrodt started noticing blood in her stool. “You don’t think it’s going to be anything serious,” she recalled. Full story on UCLA Health News & Insights
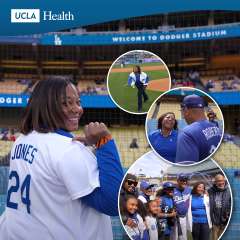
UCLA Health patient celebrates start of the 2023 Dodgers baseball season – and her good health following a game-changing colonoscopy
Angie Jones listened to her UCLA Health primary care doctor when she was told she was due for her first colonoscopy, which the U.S. Preventive Services Task Force now recommends most people get at age 45, instead of 50 as previously advised.
She is very glad she did.
During the exam, doctors found a large pre-cancerous polyp which was promptly removed, and regular monitoring continues to show no evidence of disease.
Full story on UCLA Health News & Insights

Colon cancer survivor uses TikTok to advocate for early screening
In a TikTok video with thousands of views, Elizabeth Wachsberg wears a T-shirt that reads “colonoscopy enthusiast.”
In another video, this one with 2.4 million views, Wachsberg says researchers predict colon cancer will be the leading cause of cancer deaths among people age 20 to 49 in the next few years.
After being diagnosed with stage 4 colon cancer at age 38, Wachsberg has become an outspoken advocate for early screening, posting daily videos on TikTok @mystage4story.
She talks about the symptoms that led her to get screened, her experiences with chemotherapy and the latest research on colon cancer. She answers commenters' questions, helps memorialize their loved ones lost to colon cancer and shares about the mental health challenges she experienced before and after her treatment. She also occasionally posts about her 15-year-old cat, Pete.
Full story on UCLA Health News & Insights

At 38, Brian Coyne wasn't expecting the results he received from his first colonoscopy
Brian Coyne underwent his first colonoscopy at 38, expecting to find out that his rectal bleeding was caused by nothing more serious than hemorrhoids.
Coyne still felt groggy from sedation when his gastroenterologist said he'd encountered a rectal tumor so large that he'd had to stop the procedure. “He said they found a tumor and he's 99% sure that it is cancer,” said Coyne, who lives in the Sacramento area. “You never expect to get woken up with your wife sitting right next to you and that's what they tell you.”
Coyne and his wife, Mandy, decided they would go anywhere for the best possible treatment for his stage 3 rectal cancer. Through research and a family referral, they chose UCLA Health. “I feel I have the best medical team behind me,” said Coyne, a father of two. “How else would you describe who you feel literally saved your life?”
Full story on UCLA Health News & Insights

Given 2 years to live, a patient with colorectal cancer gets his life back through a clinical trial, leading-edge technology
By all accounts, Lazaro Barajas was living a good life. At 40 years old he was married, had a good job as a general manager of a restaurant chain in Santa Clarita, and was saving to buy a first home for his family. A huge sports fan since childhood, he enjoyed attending his young son's and daughter's football and basketball games and cheering on his beloved Los Angeles Lakers.
Then, in 2019, Barajas' world was shattered when he was diagnosed with invasive colorectal cancer, a disease in which cells in the colon (the lower part of the large intestine) or rectum grow out of control.
While the majority of colorectal cancers are found during a routine colonoscopy — an imaging test for abnormalities in the colon — at 40 and with no family history of the disease, that screening wasn't on Barajas' radar. His only symptom — albeit, an alarming one — was a rapid weight loss of about 40 pounds over three weeks.
Full story on UCLA Health News & Insights
Laker for a Day- Lazaro Barajas
In May of 2019, Lazaro Barajas was diagnosed with stage-4 colon cancer. With his wife, two kids and his doctors at UCLA Health by his side, Barajas was honored at a Lakers game as Laker for a Day. He also toured the Lakers training facility, received a new jersey and attended a game.

It pays to be an advocate for your own health. Diagnosed with colorectal cancer at just 26, underscoring a troubling trend and call for more colorectal cancer screening - Kyle McEwen
When Kyle McEwen, 26, started experiencing extreme stomach pains more than a year ago, he hoped that maybe it was just the flu. But as the symptoms continued for weeks, he made an appointment with a general practitioner near his home in Thousand Oaks. That doctor concluded he was probably just suffering from anxiety and perhaps irritable bowel syndrome. "She prescribed me anti-anxiety medication and thought that was it," he said. "I admit that I have anxiety, but I did not feel like anxiety was causing my stomach issues – it didn't add up."
Determined to find answers, McEwen made an appointment with Michael Albertson, MD, a UCLA gastroenterologist who ordered a colonoscopy, a procedure that's rare for a patient so young. It turned out that McEwen had an adenocarcinoma – a malignant tumor in his rectum. “Even I could look at the images and tell that something wasn't right,” he said. “There was this black object that obviously did not belong there.”
McEwen's diagnosis underscored a trend that doctors have been tracking in recent years: More younger people are developing colorectal cancer. The problem has become so pronounced that the U.S. Preventive Services Task Force in 2021 lowered the recommended age for colorectal cancer screenings to 45. The American Cancer Society estimates there will be 106,180 new cases of colon cancer and 44,850 new cases of rectal cancer in the U.S. in 2022. Read full story on UCLA Health News & Insights
Laker for a Day- Marisa Peters
Meet Marisa Peters, wife and mother of 3, and Head of People at a new tech start-up - VideoAmp. Over a year ago, Marisa was diagnosed with stage 3 colorectal cancer following a checkup related to other health complications. With the support of her family, her organization and UCLA Health, Marisa is on her way to living her best life. Thank you for being an inspiration to us all!

Devin Dillon is the perfect example of why colorectal cancer screenings are now recommended beginning at age 45
In the first three months of 2022, Devin Dillon underwent her first colonoscopy at UCLA Health, found out she had colon cancer and learned after surgery that she was cured. Dillon, 48, credits her early diagnosis and excellent outcome to the expanded eligibility for colon cancer screening adopted last year. Guidelines in the U.S. now recommend an initial colonoscopy at age 45 instead of 50.
“I'm sort of the reason they now have the screening earlier,” she said. “It's because younger people between 45 and 50 are developing colon cancer and may not have any symptoms or risk factors.” That was the case for Dillon, superintendent of PreK-12 Operations for UCLA. “I don't have any family history of it,” she said. “I don't have any of the pre-indicators. I'm not overweight. I work out every day. I try to eat really healthy. I'm not a smoker. I don't drink. I do CrossFit.” Read From Colonoscopy to Colon Cancer Cure in 3 Months on UCLA Health News & Insights

UCLA Health patient overcame her fears to get screened for colon cancer - Gloria Riley
As a former health educator who taught the importance of early cancer screenings, Gloria Riley knew better than to put off her colorectal cancer screening. But hesitancy and the repeated urging by her primary care physician, John Mafi, MD, MPH, were initially not enough to overcome her fear of sedation, the risk of something going wrong, or the discomfort of drinking the prescribed laxative preparation solution. “It was okay for me to tell everyone else to do it, but when it came to myself, I was totally hesitant,” Riley, 56, says. “I had a big fear and I was just frozen for a long time. I wouldn't do it.”
At 35, her then-doctor recommended early colorectal screening. “My doctor was saying that as Black people, particularly as a Black woman, those tests were not designed with us in mind and so we likely needed to [be screened] sooner,” Riley recalls. “In fact, he told me that he knew of a young lady who was around my age who had colon cancer and died. But I still didn't do anything.” Colorectal cancer is the third-leading cause of cancer-related deaths. Compared to white people, Black people have a 20% higher incidence of colorectal cancer, are more likely to develop it at a younger age and be diagnosed further along in their illness.
Riley began seeing Dr. Mafi in 2016, when she was 50 years old. In the past, 50 was the recommended age to begin colonoscopy screening. New guidelines issued in 2020 have updated the age to 45. Riley shared with Dr. Mafi her fears of experiencing a loss of control from being sedated. “Gloria was very rationally worried about potential complications of the colonoscopy itself because it is an invasive procedure,” Dr. Mafi says, “Many patients have different reasons for their hesitancy. You have to really try to understand the root cause.” Dr. Mafi also highlighted the importance of trust-building. “Developing trust is not easy and takes time,” he says. “It's not something you can earn through words only, either. Our actions play an important role.”
For four years, Dr. Mafi brought up the importance of colorectal cancer screening with Riley. He made himself available to her and shared statistics and data with her. “I knew it could happen to me, but fear had a strong hold on me to where I didn't follow through” Riley says. Then in 2020, something “just clicked,” she says. Dr. Mafi's patience and urging helped Riley feel reassured and she trusted his medical advice. “I got to the point where I was afraid, but I knew I was going to go through with it anyway. I trusted my doctors.”
Gastroenterologist Wendy Ho, MD, MPH, prescribed Riley the laxative preparation drink and explained the procedure in detail beforehand, which helped assuage Riley's fears, she says. On the day of the procedure, Riley asked the nurses to hold her hand. “The anesthesiologist counted with me and the next thing I remember I was waking up,” she recalls. In that moment, Riley felt proud of herself. She was eager to let Dr. Mafi know she finally followed through with the procedure and to thank him for encouraging her to have it, providing medical data on the importance and for being so patient with her – answering all of her questions leading up to it. “I truly cannot thank him enough,” Riley says. She had put the screening off for nearly 15 years and she was finally on the other side of it.
Next came the bad news: She had a large cancerous polyp that was removed during the screening. When Dr. Mafi received a notification that Riley had undergone the procedure, he knew what a big deal this was for her and sent her a note to ask how she was feeling. “She wrote back right away and mentioned she was appreciative of my urging because they did end up finding a high-risk adenoma (polyp),” Dr. Mafi says. “I was really happy to learn she had been screened and had the polyp successfully removed. Had she not, the conversation could have instead been about her cancer spreading.” Riley says if she could go back in time, she would have had the screening, “a lot sooner.”
“I could have full blown cancer right now,” she says. “I think about it all the time. And right after [my procedure] is when Chadwick Boseman died. He was a lot younger than me.” Six months after the surgery, Riley had another screening. “I wasn't as afraid as I was the first time,” she says. There were no signs of cancer. Her next screening will take place in five years.
Riley has advice for other patients: Don't wait for symptoms to develop because it could be too late. “It doesn't matter if you eat healthy or not. It doesn't matter if no one in your family has ever had it. It doesn't matter what type of lifestyle you're living. It's still important to get screened because you could be the first in your family.”

Ready for "all clear" - Porchia Toussaint
“My dad was 54 years old when he passed away,” says Porchia Toussaint, who was 31 when she learned her dad had stage 4 colon cancer. “His doctor told my brother and I that because we were his kids, we needed to get follow-up colonoscopies. I had no idea what a colonoscopy was. It was an interesting process. The actual procedure was fine. They put me to sleep and when I woke up the doctor said, ‘You did great. We didn't find anything.' They found two polyps in my brother, which they removed.”
Polyps in the colon can potentially become colon cancer. “They said to repeat getting a colonoscopy every five years,” Toussaint says. “It's preventive care, since colon cancer is slow-growing. My brother and I now go for regular colonoscopies. I think you should get tested, especially if it runs in your family. I have my colonoscopy next week and hopefully, they say it's all clear and to come back in five years.”

Listen to your body - Cameron Kalunian
“I was 35 years old when I started seeing some blood in my stool,” says Cameron Kalunian, whose primary care physician sent Cameron to a gastroenterologist to determine the cause. “They performed a sigmoidoscopy, which is a less invasive test than a colonoscopy. They found a large tumor at my colorectal junction.”
Kalunian underwent colorectal surgery in late 2019, with Jonathan Sack, MD, who found a tumor and treated it. Kalunian was declared in remission within a month.
Because Kalunian took quick action upon seeing symptoms, his colon cancer was identified in stage 1.
“They did my surgery laparoscopically, so I only have a tiny scar on my abdomen. I was impressed with how cutting-edge all the technology at UCLA Health was,” he says. “My anesthesiologist, rather than putting me on a morphine drip or IV for pain medication, gave me a spinal tap. So I had a lesser dosage of medicine, which meant I was less likely to have complications. I was home three days after the surgery and was back at work within two weeks of my surgery. Every aspect of the care I received was thorough and reassuring. I felt the comprehensive care and felt that my interests were being taken care of.”
Initially, Kalunian says, he assumed because he was young there was no way he could have colon cancer.
“I didn't have a family history, but I had seen in the media that there is a higher prevalence of early-onset colon cancer,” he says. “I think there are a lot of stigmas associated with the testing. Ultimately, it wasn't a big deal. I think, now, I've had four colonoscopies and you get better at it each time. You know what to expect and it's not scary. The most important thing is, if you have symptoms to follow up on them. Listen to your body. Blood in the stool is something to pay attention to and take very seriously.”

Just do it - James Weatherall
“My new primary care physician was shocked that I hadn't had a colonoscopy yet,” admits 62-year-old James Weatherall. James chose UCLA Health for his medical care after moving to Los Angeles. “I went in for my colonoscopy, expecting nothing, but came out of it with a tumor. My whole world changed. It was a T2N0 [Stage 2 tumor with zero evidence of spread to lymph nodes] but after a biopsy, they upgraded it to a T3, meaning it was larger than they originally thought. It was pure luck that the cancer had not spread to my lymph nodes. Dr. Anne Lin, my surgeon, was wonderful. She removed 14 lymph nodes to ensure there was zero trace of the cancer left. She was able to do this very complex surgery laproscopically with minimal scarring. It was amazing. After the surgery, Dr. Lin gave me the option of pursuing chemotherapy as an extra precaution step. I met with Dr. Joel Hecht who recommended chemotherapy pills. As he described it, 'it was chemo with a small c, not chemo with a big C'.”
James took medication for six months before undergoing a CT scan. Sighing with relief, he says, “It showed no signs of lingering cancer! While I was technically in remission, they said I should have only a small party. I'll have to return every six months for new CT scans. If after three years my scan is still clear, then I should have a little bigger party. If after five years my scan is still clear, then I should throw a big party! In my book, I owe it to my primary care physician, Dr. Benjamin Waterman for pressuring me to get my colonoscopy. Had I continued to procrastinate, I don't know how quickly my tumor would have grown. Every time I meet my contemporaries, I'm not shy about talking about colonoscopies. I didn't have any symptoms, so my colonoscopy was considered a screening test. From that standpoint, it was a successful screening. It saved my life. When your doctor tells you it's time for a colonoscopy, just do it.”

Ride on - Stephane Strouk
“I was one hundred percent sure I had hemorrhoids,” recalls Stephane Strouk, an avid motorcyclist who decided to get a colonoscopy in 2016 to be sure. “I woke up, and the doctor said I had stage 3C colorectal cancer. I did 37 radiation treatments, five treatments per week. You meet wonderful people at radiation, and you see the advances in technology. They were pinpointing my tumor, and it worked. The tumor shrunk 40%, and my doctor was able to do the surgery, remove the tumor, and part of my colon. I was also doing chemotherapy in Santa Monica. It was difficult, but it was the coolest place on Earth. You go in and you're facing the sea. You see the ocean and the palm trees and the blue sky. It feels like a five-star hotel. It was very relaxing and quiet. My whole team was the greatest, from the nurses to the doctors. They all become your friend in the end. They're very human. They care.”
After a successful colorectal surgery, Stephane resumed life with an ostomy bag. He reveals, “The ostomy bag was the most difficult part for me. I'm on a motorcycle every day, no matter what. I have different motorcycles, and some of them I couldn't ride because the bag would explode. I was back on my bike 10 days after my surgery. I went to radiation with my bike as much as I could. After seven or eight months, they removed the ostomy bag and reattached everything. It took maybe a year to adapt, but now everything is working. It's wonderful. I live every day. I wake up in the morning, see the blue sky, ride by UCLA Health and thank my doctors. They made everything so easy.”

The home FIT test led to a colonoscopy and a new appreciation for colorectal cancer screening - Fuad Afifi
The 60-year-old retired chef typically prefers to be more private, but he's opening up about the importance of cancer screening after losing his sister to the disease earlier this year.
“She was in her early 60s,” he says. “A very vibrant, outgoing person. Very athletic.” They had no family history of colorectal cancer, he adds. Colorectal cancer is the third most commonly diagnosed cancer in men and women in the United States. The American Cancer Society estimates nearly 105,000 new cases of colon cancer and more than 45,000 cases of rectal cancer will be diagnosed in 2021.There are often no symptoms of colorectal cancer until the disease has progressed. “If you don't feel symptoms, you think that you're OK,” Afifi says.
Before undergoing his first colonoscopy this year, Afifi previously opted for the fecal immunochemical test, or FIT, a non-invasive at-home test that requires laboratory submission of a tiny stool sample to be analyzed for traces of blood. The FIT must be performed annually. “It's better to have any screening as opposed to no screening,” says Kevin Ghassemi, MD, a gastroenterologist with UCLA Health. “The fecal immunochemical test is a very reasonable test to look for blood in the colon, which, if present, will highlight the need for colonoscopy.” Afifi did the FIT in 2018 and again in 2020. The first time, the results were negative for blood. But last year, they came back positive, indicating further exam was needed.
Around the same time, his sister died. “She was diagnosed six months ago and it had already metastasized to the liver,” Afifi says. “That gave me a clue. It helped me put some sense into it. And I decided I really wanted to do the colonoscopy.” Colonoscopy requires dietary preparation beforehand to clean out the colon and sedation during the procedure. The exam uses a tiny camera on a scope to view the colon and remove any polyps, which are growths on the colon lining that can sometimes become cancerous. Polyps do not generally cause symptoms, Dr. Ghassemi says, and they don't always bleed, “which is why the stool test does have some limitations.” In Afifi's case, though, the FIT led to a colonoscopy, which in turn led to the discovery of polyps. “It was really a blessing that he decided to get this form of screening,” Dr. Ghassemi says. Dr. Ghassemi removed five pre-cancerous polyps during Afifi's exam.
“I'm glad I did it,” Afifi says. “That's what I know.” Now that he's experienced a colonoscopy, Afifi calls it “a very simple procedure.” “It opened my eyes, actually,” he says. “Because a lot of people don't want to do it, either because of some personal reason or they don't want to drink the things to clear the colon. People might consider colonoscopy an invasive surgical procedure or a personal thing, and there's a lot of people who don't want to expose themselves to that.”
Despite evidence that screening reduces colorectal cancer cases and deaths, screening participation in the U.S. among adults 50 and older was only 67% before the pandemic, with even lower rates among people of color. Rates of colorectal cancer are higher among Black Americans than among whites. Black people are 20% more likely to be diagnosed with the disease and 40% more likely to die from it. Current recommendations call for screening to begin at age 50, though the U.S. Preventive Services Task Force is recommending the age be lowered to 45 due to an increased incidence of colorectal cancer in younger people. Those with a family history of the disease should begin screening even earlier.
For those hesitant to have a colonoscopy, the FIT might be a good place to start, Dr. Ghassemi notes. But Afifi now swears by the more thorough exam. “It's awareness,” he says. “You have to be aware of your body. And you have to remove the fear. I'm not afraid of dying, but I am afraid of not taking the right precautions and doing what's necessary to keep this body going.”
Afifi says he hopes sharing his experience might prevent others from needlessly suffering the loss of a loved one, as he did with his sister. “I think she died unnecessarily,” he says. “I am doing this in her memory, because if I can save one life with my story, it means we save humanity.”
Keeping you connected through post-surgery app - Anne Lin, MD
“I focus a lot of energy on treating the patient as a whole person,” explains Dr. Anne Lin, a colon and rectal surgeon at Ronald Reagan UCLA Medical Center. “When I meet patients, often they already have the diagnosis of colon cancer. I talk to them about the next steps in their care. I tell them about the operation and what care will be like during their hospitalization and after their surgery. We have been using an app to help patients with their transition out of the hospital. We try to connect with patients with us during this vulnerable post-discharge time using a remote monitoring application.”
Dr. Lin developed the monitoring app with UCLA Health as a way to allow patients to send messages directly to their physician. She further explains, “We, the doctors, curate the questions sent for that particular patient and their problems. The patients have daily tasks, they can take photos of their wounds, and we are alerted of any early warning signs of an infection. The goal of the app is to enable patients to be more active participants in their care. It helps patients be more comfortable with the entire recovery process, and they're empowered to improve their health. We've dramatically reduced emergency department visits and readmissions through the use of this app. It's been a really wonderful thing because the patients feel connected to us. I feel like I have an understanding of where my patients are, and it helps me feel more comfortable about releasing them. In a hospital, they're monitored really well, but then they go home and there is no monitoring. Knowing there will continue to be an exchange makes me feel very comfortable.”

Second opinion helped save my colon - Linda Kama'ila
“I went in for a routine colonoscopy, but the doctor was unable to remove a certain polyp, so they sent me to a surgeon who wanted to remove one-third of my colon,” recalls 64-year-old Linda Kama'ila, who immediately looked for a second opinion. “I would have been out of work for six weeks with two major surgeries. I try really hard to stay healthy, and being out of work for that long with lifelong consequences was really concerning. Online, I saw that UCLA Health offered a mucosal resection procedure. Dr. Danny Issa offered this outpatient procedure, and he got the benign polyp out. It was a great success and I got to keep all of my functioning. It was all done in two afternoons. UCLA Health's quality can't be beat because the staff is research-oriented. Dr. Issa's work—which he's still publishing-- shows that when there's a history of benign polyps, there isn't always a reason to do a major surgery as if the polyp is cancerous. I would have lost one-third of my colon for something that was not malignant. I'm so grateful to UCLA Health. It couldn't have been a better experience.”

Any dietary and lifestyle changes a patient is willing to make can be hugely beneficial to their health - Nancee Jaffe, MS, RDN
“Dietary and lifestyle interventions can make a huge difference in colorectal cancer prevention,” explains Nancee Jaffe, lead dietitian at UCLA Health Digestive Diseases. “We've learned that 60% of colorectal cancer deaths could have been prevented by screening and lifestyle changes. Our hope is that by talking about screening practices and nutrition and lifestyle interventions, we can actually stave off this disease. Not exercising, drinking alcohol in more than moderation, smoking, and low amounts of fiber-rich foods are all problematic and can lead to colorectal cancer. Eating lots of fruits and vegetables, whole grains, beans, legumes, nuts, and seeds are good interventions. It's not all or nothing. Any amount counts. Any difference a patient is willing to make will be hugely beneficial to their health.”

Removing early colon cancers endoscopically - Adarsh M. Thaker, MD
“I don't do a lot of screenings because, in the majority of my colonoscopies, I've been referred to remove a polyp,” states Dr. Adarsh M. Thaker, an interventional endoscopist at UCLA Health. “We remove large polyps and even early colon cancers endoscopically, to prevent them from either turning into worse cancer or in order to avoid surgery. We put so much attention on polyps and colonoscopies because a polyp is a precancerous lesion. That means if you leave it be, in five or ten years, a significant number of polyps turn into colon cancer. In general, any polyp that has a biopsy that does not show cancer is still worth an endoscopist taking a look at it. We might be able to remove it in a low-risk, same-day procedure. In fact, our surgeons often send their patients to one of us to remove the polyps before they will consider doing surgery. I like the procedural aspect of telling a patient I was able to remove it all and that they are good to go.”

You'd be crazy not to start colorectal cancer screening - Walter Fraser
“My brother's wife died from colon cancer, and her experience was the opposite of mine,” remarks Walter Fraser, a patient who recently had a colonoscopy at UCLA Health Burbank Primary & Specialty Care. “She never got a colonoscopy until one day she woke up and was diagnosed with stage four colon cancer. I started getting colonoscopies 20 years ago, and they were uneventful for 15 years. Then, they began seeing polyps. I had several large polyps, which they removed, and one that was lying flat, which was likely to develop into a cancerous polyp. They removed it, and everything was fine from my patient perspective. I wouldn't even have known I had a procedure except for the fact that on paper, I knew I had. I'm always very happy with the treatment I get here. I can't recommend the whole UCLA Health group or getting your colonoscopy highly enough. You'd have to be crazy not to start getting tested like they recommend.”

A small price to pay - Tina Storage, MD
"In residency, I changed my focus from oncology to gastroenterology. Instead of being on the treatment side, I could now be on the prevention side,” reveals Dr. Tina Storage, a UCLA Health gastroenterologist. “There was an 18-year-old who had severe anemia secondary to colon cancer. She had ulcerative colitis, so she should have been screened for colon cancer, but she wasn't. I was really heartbroken that she was so young and passing from this preventable disease. If colon cancer is detected at a localized stage, a person's survival is upward of 90%. If we can detect precancerous polyps before they even turn into cancer, we can prevent the diagnosis. A colonoscopy feels like a small price to pay to change the alarming statistic of 50,000 people dying of colon cancer in 2019.”

An Uncommon Bruin - Fola May, MD, PhD, MPhil
Dr. Fola May, UCLA physician and research, was recognized as an Uncommon Bruin by UCLA Athletics for her work on raising awareness about colon cancer risk and screening in the field of gastroenterology. She took the opportunity at the women's basketball game on March 1, 2020 to remind everyone that colon cancer the third most common cancer in the U.S. but screening for colon cancer reduces the number of cases, prevents deaths from colon cancer, and allows doctors to detect colon cancer early when treatment is more likely to be successful. From the research lab, to the clinic, to the community, Dr. May is a champion for colon cancer prevention and awareness. An Uncommon Buin!