For men facing prostate cancer, knowing exactly where the disease lies can make the difference between a targeted treatment and a more invasive procedure. At UCLA Health, researchers are harnessing artificial intelligence to map tumors more precisely, helping physicians better diagnose the extent of disease, identify candidates for less-invasive treatments and plan more precise treatments.
In a series of new UCLA-led studies, investigators have made significant advancements in developing an AI tool, called Unfold AI, which combines MRI data with biopsy results to generate a detailed, 3D map of where cancer sits inside the prostate. The technology, developed in partnership with the UCLA-backed startup Avenda Health, is designed to give physicians a clearer picture of tumor size and boundaries, providing new insights for making informed treatment decisions.
“Overall, the use of AI in cancer treatment could lead to more effective and personalized care for patients, with treatments that are better tailored to their individual needs and more successful in fighting the disease,” said Wayne Brisbane, MD, assistant professor of urology at the David Geffen School of Medicine at UCLA and member of the UCLA Health Jonsson Comprehensive Cancer Center.
Here’s a look at some of the most recent UCLA-led studies showing how AI is helping to advance more precise and personalized treatment strategies for prostate cancer.
Predicting who will benefit from focal therapy
In one study published in BJUI Compass, Dr. Brisbane and his colleagues used Unfold AI to see if it could help doctors identify who is most likely to benefit from partial gland cryoablation, a minimally invasive procedure that freezes and destroys only the cancerous part of the prostate.
Partial gland cryoablation, a type of focal therapy, aims to destroy cancer cells while sparing healthy tissue, reducing side effects compared with surgery or radiation and improving quality of life. The procedure uses imaging guidance, such as MRI, to locate tumors and deliver energy precisely to the affected area. However, current methods often underestimate tumor size and can miss smaller cancer spots, leading to incomplete treatment and recurrence.
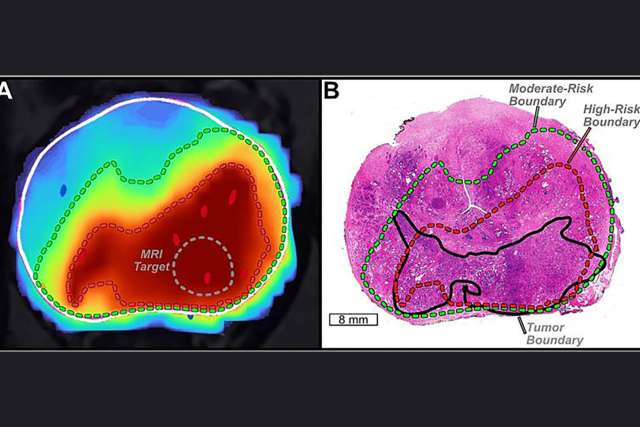
Unfold AI addresses this limitation by analyzing MRI and biopsy data to generate a detailed, 3D map of the prostate tumor. In a clinical trial of 204 men who underwent partial gland cryoablation at UCLA between 2017 and 2022, physicians used the AI tool to estimate tumor volume and compare it with traditional indicators, including tumor grade and PSA levels.
The study found that tumor volume was the strongest predictor of treatment success. Men with tumors smaller than 1.5 cubic centimeters were far more likely to be cured and avoid additional treatment or metastases. Using this tumor volume threshold as a criterion could have prevented 72% of treatment failures, the researchers reported.
“This is important because tumor volume is a major determinant of treatment success or failure. Using AI to predict tumor volume and shape gives a clearer picture and could help choose better candidates for focal cryotherapy,” said Leonard Marks, MD, professor and deKernion Endowed Chair in Urology at the David Geffen School of Medicine at UCLA, member of the UCLA Health Jonsson Comprehensive Cancer Center, and senior author of the study.
Improving prostate cancer outcomes
A second study, published in the Journal of Urology, shows that AI can help doctors more accurately identify the extent of prostate cancer, potentially improving diagnosis, treatment planning and surgical outcomes.
The Unfold AI system was found to define the boundaries of cancerous tissue far more accurately than conventional methods, making predictions of tumor size 45 times more precise than doctors’ assessments alone.
Accurately mapping tumor extent is essential because different stages require different approaches, including active surveillance, surgery, focal therapy, radiation, or systemic treatments. Traditional methods rely on MRI and PSA levels, but some tumors can be “MRI-invisible,” leading to underestimated tumor size. AI addresses this by more precisely defining tumor margins, which is especially valuable for focal therapy.
Researchers tested the system in a multi-reader, multi-case study with seven urologists and three radiologists reviewing 50 patient cases. Initially, physicians manually outlined suspected cancer areas on MRI. Weeks later, they re-evaluated the same cases using AI assistance. Using conventional methods, physicians achieved a negative margin, or complete tumor coverage, only 1.6% of the time. With AI, this increased to 72.8%. AI also improved clinician consistency and increased recommendations for focal therapy, potentially reducing side effects from more aggressive treatments.
AI more accurately predicts prostate cancer spread to seminal vesicles than MRI
The third study evaluated Unfold AI’s ability to predict seminal vesicle invasion, the spread of cancer from the prostate into the seminal vesicles, which is a critical factor in staging and treatment planning. MRI often misses seminal vesicle invasion due to resolution limits and variability among readers, but AI-generated cancer maps successfully identified seminal vesicle invasion even without specific training for this task.
Researchers analyzed two cohorts: 147 prostatectomy patients from a single institution and 20 patients from a second institution, half of whom had confirmed seminal vesicle invasion. Using 3D cancer estimation maps generated from preoperative imaging and clinical data, AI predictions far outperformed MRI. In the first cohort, MRI missed 48% of seminal vesicle invasion cases, while AI missed only 8%. In the second cohort, MRI missed 40% of cases compared with 20% for AI.
“These findings suggest that AI could significantly improve the preoperative detection of seminal vesicle invasion, supporting more accurate staging and treatment planning for prostate cancer,” said Dr. Brisbane. “The results highlight AI’s potential to complement MRI and provide more reliable guidance for surgical and radiation strategies.”