In Alzheimer’s disease, memory loss and dementia result when neurons die and critical brain connections are damaged. But understanding the disease will take more than just learning how neurons die. Over the last 5 years, scientists have discovered that immune cells in the brain also help drive dementia. Now, a new study led by researchers at the David Geffen School of Medicine at UCLA reveals another layer of complexity to the ways immune cells and neurons interact.
“Our study shows for the first time how complex and time-dependent these interactions are,” said Daniel Geschwind, MD, PhD, the Gordon and Virginia MacDonald Distinguished Professor of Neurology, Psychiatry, and Human Genetics at UCLA and the paper's senior author.
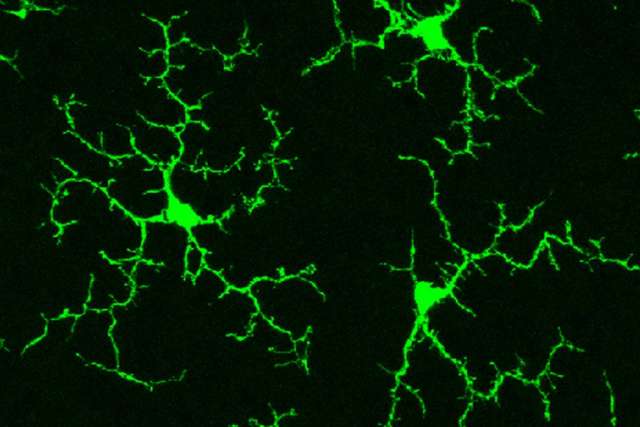
In addition to neurons, the brain contains immune cells called microglia, which clean up cellular debris, fight infections, and ignite inflammation as needed. Recent findings had suggested that Alzheimer’s disease damages the brain when overactive microglia cause too much inflammation. This inflammation damages the synapses, or the connections between neurons, cutting off their ability to communicate.
The new results, published in the journal Cell Reports, show there’s much more to the story. By analyzing patterns of gene expression throughout different time points in a mouse model of the disease, first author Jessica Rexach, MD, PhD, an assistant professor of neurology, discovered something unexpected. Rather than the simple overexcitement of microglia, as was previously thought, the new data reveal a push and pull of opposing forces.
“It’s not a single trajectory of increasing inflammation, but a complex interplay of factors that changes over time,” said Rexach.
Early on in disease, inflammation does flare up; but then it’s tamped down. While this prevents runaway inflammation, it also hinders important immune defenses. For instance, one function of microglia is cleaning up unneeded proteins and debris. A hallmark of Alzheimer’s disease is the buildup of tangled masses of a protein called tau. If microglia are suppressed, tau tangles may accumulate unchecked in the brain, causing dementia.
This finding suggests that timing may have a significant effect on whether a therapy works.
“Many drugs that people were thinking about moving into trials actually suppress the immune response, because people are trying to be anti-inflammatory,” Geschwind said. “But maybe you want to have a little more immune activation at certain stages of disease. There’s a careful balance, and we’ve elucidated that.”
Normal aging generally leads to a more lackluster immune system, and age is a key risk factor for most neurodegenerative disorders, such as Alzheimer’s disease. Immune suppression is a known feature of aging; now it appears to be an important driver of disease.
The gene expression pattern seen here resembles what happens in response to chronic viral infections, Dr. Rexach said. A possible instigator for that activity is loose pieces of RNA resulting from damage caused by tau tangles. Those RNA fragments look like viruses, and confuse the microglia into suppressing important defense strategies.
Runaway inflammation can cause widespread damage in the body, so the immune system deploys a complex array of feedback systems to keep that from happening while still effectively killing the virus. In the case of Alzheimer’s, however, there is no virus, and stifling the activity of microglia may be more harmful than helpful, as tau protein debris accumulates.
To test their model, the researchers used a new technique called chemical genomics, in which drugs are given that mimic the effect of gene expression changes. By recreating the gene expression changes they observed, they successfully altered the effects of microglia on nerve cells in the predicted pattern. By that token, medications could potentially also counteract the changes associated with dementia, reactivating the microglia and clearing out the tau tangles. “We use a chemical genomics approach to identify drugs that would be predicted to reverse the changes we see,” said Geschwind.
As the population ages, the rate of Alzheimer’s disease continues to rise, with more than 5 million people currently living with the disease. To date, no drugs have been approved to slow down or reverse the ongoing cognitive decline of Alzheimer’s disease. Studies like this one that unveil the complex factors at play in the brain will help identify how drugs can thwart the progression of the disease.
“Finding therapies for dementia is a major public health priority,” said Geschwind. “To find therapies, we need to know what’s going on. We need to find the disease mechanism.”
Caroline Seydel is the author of this article.