The baby girl was in and out of the intensive care unit at the UCLA Mattel Children’s Hospital since she was a few days old. A mechanical ventilator helped her breathe and she was mostly sedated to keep her from tugging at the multiple lines, monitors and electrodes connected to her tiny body. She was waiting for a heart transplant.
Her doctor, Marlin Touma, MD, PhD, consulted with her family throughout the baby’s stay. And when the baby was a year old, a donor heart was located and the transplant surgery was a success. But Dr. Touma’s work with the defective heart was only beginning.
The baby was born with Primary Endocardial Fibroelastosis (pEFE), a congenital defect in which the lining of the heart muscle thickens. Soon after birth, babies with pEFE experience a complete failure of the heart’s left ventricle. The only treatment is a heart transplant.
“We treat many patients who have different congenital heart defects, but this [defect] was very striking to me,” said Dr. Touma, associate professor-in-residence in pediatrics at the David Geffen School of Medicine at UCLA. “And unfortunately, we don't have a specific, targeted therapy.”
Dr. Touma is a physician-scientist and director of the UCLA Congenital Heart Defects Research Program. In a “Bedside-to-Bench” research model, she incorporates her clinical work into the laboratory by investigating how different mechanisms of genetic regulation can lead to a range of heart defects.
Affecting about 1 in 100 babies, congenital heart defects are the most common congenital disorders. They range in severity. A hole in the heart is a relatively mild condition. An extreme is hypoplastic left heart syndrome: large structures on the left side of the heart are underdeveloped or missing. Congenital heart defects are also the most common birth defect-related cause of death in the pediatric population.
The hope is that by further understanding the underlying mechanisms of the tiny, growing heart, Dr. Touma and her team at the Touma Lab can identify novel treatments.
Understanding physiology
There are many reasons why a baby may develop a heart defect.
“It's multifactorial but I will say we know very little,” said Dr. Touma. “We know that genetics contribute to congenital heart defects. And that could be a single gene mutation or more than one gene.
“Sometimes that susceptibility, along with other factors such as smoking, vitamin deficiency, alcoholism or maternal diabetes, could evolve into a congenital heart defect.”
Fetal echocardiography or a cardiac MRI can help diagnose defects in utero, and surgical procedures have advanced considerably post-birth. But unlike adults, extensive clinical trials and drug development are lagging for babies.
“Our medical treatment is what we need to work on,” said Dr. Touma. “And we will not be able to work on that unless we understand the exact physiology of the heart that's already malformed at the cellular level. We cannot identify preventive strategies or make a significant and sizable impact on patient care unless we fully understand the roots of the problem.”

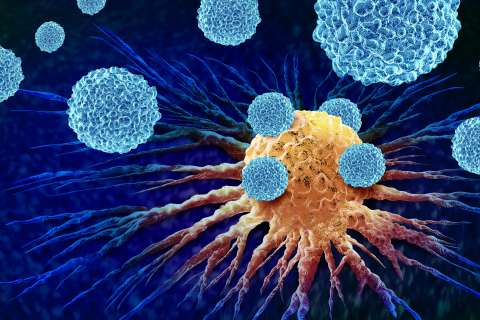
The Congenital Heart Defect-Bio Specimen Resources Core, established in the Touma Lab, bridges clinical work and research. Through campus-wide collaboration with other clinicians, including surgeons, geneticists, pathologists and cardiologists, the UCLA CHD-BioCore stores blood and tissue samples from babies and their family members. These samples are indexed by type of heart defect and complete clinical history, along with the genomic datasets. The Core also houses stem cells (iPSC) derived from patients.
“This resource is a biobank of tissue and iPSC that we can also share with the scientific community,” said Dr. Touma. “When you have the resources, you are more interested to interrogate the question – so now more people are engaged in these endeavors to study the mechanisms of congenital heart defects, and why things that we know work in adults may not work in children.”
In the baby girl’s case, Dr. Touma’s team obtained tissue from her defective heart and blood samples from the baby as well as from her parents to study the genetic basis for pEFE.
They discovered that a rare recessive variant of the cilia gene that codes for the ALMS1 protein underlies pEFE. The researchers then generated stem cells from pEFE patients, and reprogrammed and differentiated them into cardiomyocytes, the cells in the heart muscle that allow it to contract.
“The new cardiomyocyte will carry the same mutation – and you can then study it at the bench and understand how this mutation resulted in the defect,” said Dr. Touma. “And if this mutation affects a gene that's involved in an important pathway, you can tell how this patient needs to be treated, to bypass this limitation.”
Dr. Touma kept in touch with the family, and several years later saw the little baby she once treated. Though her genetic mutation had affected her vision, and she was short for her age, the vibrant child was doing well with her transplanted heart.
Genomic studies
Dr. Touma and her team are also focusing on other genetic factors, including the role of a specific type of RNA: long non-coding RNA (lncRNA). These are lengthy strands of genetic code that regulate gene activity in various ways.
“If we look at all the genomic studies that have been done on congenital heart defects until now, I will say less than 30 percent are found in protein-coding genes,” said Dr. Touma.
“We know a number of lncRNAs are important in cardiac development and in stem cell differentiation, but we don't know that much about how they are involved in congenital heart defects.”
Most recently, Dr. Touma’s team discovered that a specific lncRNA complex is involved in the early stages of muscle cell development, including cardiomyocytes. It also interacts with important components on the membranes of the cell. The researchers are now examining the value of this lncRNA as a possible therapeutic target to improve cardiac muscle function and integrity in babies with single ventricle heart disease.
“The discovery part is very rewarding,” said Dr. Touma. “If we are studying something that was unknown in the past, the potential of this new discovery will be very high –because it may result in a paradigm shift or completely change the field.”