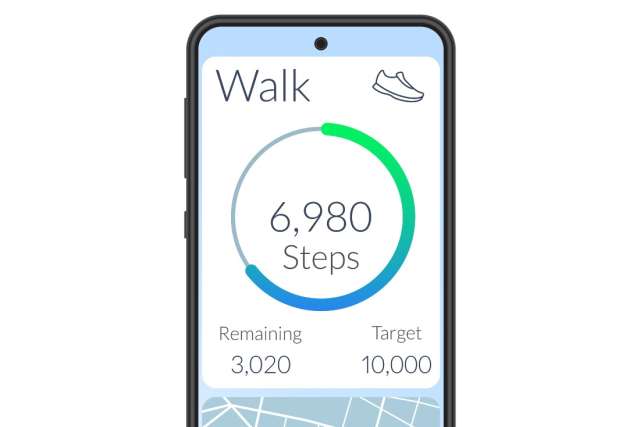
Taking a certain number of steps for just a few days per week can significantly improve your cardiovascular health according to a recent UCLA Health study.
The research, overseen by Beate Ritz, MD, Vice Chair of Epidemiology at UCLA, and analyzed by one of her former doctoral students Dr. Inoue, an Assistant Professor at Kyoto University, suggests that adults who find it difficult to exercise regularly can still reap health benefits by walking the recommended number of steps (8,000) for only a couple days out of the week.
The cohort study was comprised of 3,101 consenting adult participants from the 2005-2006 National Health and Nutrition Examination (NHANES) surveys, a sample representative of the US population. All participants, ages 20 and up, were placed into three groups according to the number of days per week they reported taking 8000 steps or more: 0 days, 1-2 days, and 3-7 days, and followed for mortality until 2019. For step count data collection, participants wore accelerometers, monitors that determine when a person is engaged in physical activity.
According to Dr. Ritz, the findings are important.
“If you take 8,000 steps or more at least one to three times a week, then your likelihood of dying is reduced by 14%,” she said.
Thus, adults who find it challenging to exercise regularly can still achieve meaningful health benefits by doing one of the simplest exercises - walking.
“What we were trying to figure out is: what is the lowest limit of exercise a person can do and still see a benefit? Especially for the elderly who may not be able to get the 8,000 steps in every day,” Dr. Ritz said. “We were also thinking about older employed people who don’t have sufficient time to exercise regularly.”
Dr. Ritz suggested that, even if those with busy schedules are able to get outside and walk on the weekend or during their days off, the exercise would be significantly helping them improve heart health.
Of the entire group, 632 participants did not take 8000 steps any day of the week (0 days), 532 participants took 8,000 steps 1-2 days out of the week and 1937 participants took 8,000 steps 3-7 days out of the week. Percentages were scaled according to the number of participants in each group.
Over the course of the 10-year follow up, there were 138 cardiovascular deaths (5.3%) and 439 all-cause deaths (14.2%) among the participants. Researchers found that the all-cause mortality and cardiovascular mortality risk was lower among participants who walked 1-2 days per week and among those who walked 3-7 days per week compared to the “0 day” group who did not take the 8000 steps during anytime of the study. Those in the “3-7” group had only a slightly lower mortality risk than those in the “1-2” despite having three times the number of people in that category.
Factors impacting results
Dr. Ritz explained that there were dynamics within the study that could have affected some of the study’s validity.
For example, “if you have a baseline measure of physical activity and you follow people all the way to their deaths, chances are there were people who were already had been reducing their step count because they were not doing well physically,” Dr. Ritz said.
Other factors played a role like older age, obesity, and whether participants smoked or used particular statins for illnesses diagnosed prior to the beginning of the study.
In addition, the study showed those taking 8,000 or more steps per day were younger, predominantly men, Hispanic, insured, married, did not smoke, and had little-to-no comorbidities (i.e. hypertension, cancer, or cardiovascular disease).
Dr. Ritz shared that though this data had some limitations, there were also some advantages that allowed this study to give a clearer view of physical activity and its impact against cardiovascular disease than previous studies.
One was that the participants were relatively diverse when it came to race. Also, gender participation was nearly even, with 49% of the participants being men (1,518) and 51% being women (1,583).
The other advantage was that the technology used gave researchers better readings on when participants were active and when they were resting.
“It’s been proven in other studies that physical activity is protective against cardiovascular disease risk, but what’s different and new in this study is that we had accelerometers, devices used to record rest and recovery,” said Dr. Ritz.
“This study relied on a representative group of diverse people from the U.S. who were invited and chose to do this study not because of disease.”