Researchers at UCLA Health have developed a blood test that can distinguish between two very similar movement disorders, Parkinson’s disease and multiple system atrophy (MSA). The test, which is currently for research use only, identifies the disease by analyzing the contents of tiny sacs called “exosomes” that are sent out by brain cells and wind up in the blood.
The researchers report their findings in this month’s Acta Neuropathologica.
Parkinson’s disease can be difficult to distinguish from other neurodegenerative diseases, including MSA, due to similar symptoms such as muscle rigidity and tremors. Patients who have been incorrectly diagnosed with one or the other disease may feel anxiety when unexpected symptoms occur, or, in the case of a Parkinson’s misdiagnosis, the disease progresses faster than predicted.
“If they do have Parkinson’s, there are a lot of treatments that can help with the symptoms for a long time,” says Gal Bitan, professor of neurology at the David Geffen School of Medicine at UCLA. “If they have MSA, which is a very aggressive disease that leads to rapid deterioration, they would want to prepare. They would want to talk with loved ones, and possibly take care of their estate.”
Also, inaccurate diagnoses can skew clinical trial results. “If you’re enrolling the wrong people in clinical trials, the likelihood of the treatment to work is much lower,” says Bitan. “You’re going to get people in which the treatment didn’t work, and they count as negative, but it didn’t work because they didn’t have the disease the treatment was meant for.”
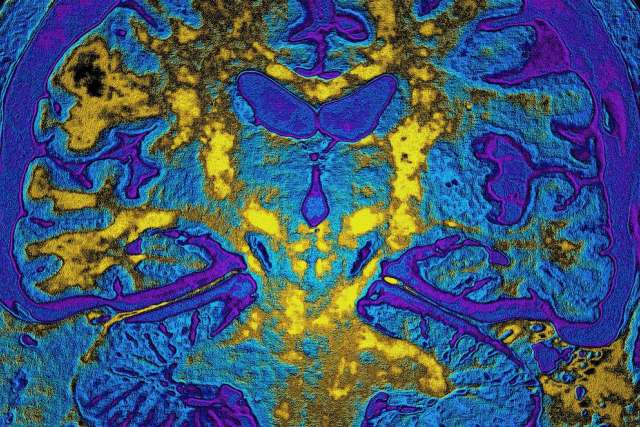
Instead of relying on symptoms, which can be highly variable and ambiguous, doctors would rather see what’s happening in the brain in order to make a diagnosis. Both Parkinson’s disease and MSA are associated with buildup of a protein called alpha-synuclein, but there are no good ways to look for the protein in a living brain. Imaging procedures, like MRI, are expensive and can’t directly detect alpha-synuclein. Sampling the cerebrospinal fluid can reveal changes in the levels of alpha-synuclein, but the test involves a needle in the spine, which patients often prefer to avoid. A blood test that can detect changes in the brain would solve a lot of these problems.
It turns out that brain cells, like other cells around the body, release miniature sacs full of chemicals, called exosomes. “We think the cells use them like a message system,” Bitan explains. “They can be taken up by other cells, and the cells can read that chemical message and know they need to respond in a particular way.” Not every exosome that’s released gets picked up, however, and some of these make their way into the bloodstream.
Several years ago, it was discovered that exosomes coming from the brain in the blood of Parkinson’s patients carried high levels of alpha-synuclein. In both Parkinson’s disease and MSA, excess alpha-synuclein builds up in clumps, causing damage to brain cells. A key difference between the two diseases is where that alpha-synuclein builds up. In Parkinson’s, the clumps arise in neurons, while in MSA the deposits are in another type of brain cell, called oligodendrocytes.
In both cases, as alpha-synuclein builds up, the cells try to cast off the surplus protein by sending it out of the cell in exosomes. In the trial, analyzing the alpha-synuclein concentration in exosomes from neurons and oligodendrocytes allowed researchers to successfully distinguish between patients with Parkinson’s and those with MSA (and those in the healthy control group).
Both Parkinson’s and MSA patients had elevated alpha-synuclein, but in Parkinson’s it mostly came from neurons, while in MSA it came from oligodendrocytes. The researchers could tell the two diseases apart with high accuracy.
“This is a major breakthrough, because it allows us to analyze what’s going on in the brain using a blood test,” Bitan says.
That discovery was just a first step, however. Bitan and his colleagues spent 5 years meticulously standardizing and calibrating the test to ensure that they were collecting the exosomes using a reproducible method, and that the exosomes were categorized correctly.
They noticed, for instance, that alpha-synuclein levels in samples collected from different clinics varied quite a bit. These differences didn’t reflect an inherent difference in the study populations, but were simply due to differences in the laboratory procedures. “Little differences in the method matter a lot,” Bitan says. To smooth out those differences, instead of classifying patients by the absolute amount of alpha-synuclein, the researchers calculated the ratio of alpha-synuclein in exosomes that came from neurons versus oligodendrocytes.
“Using the ratio helped a lot with normalization of the data and eliminating site-to-site differences,” Bitan says.
Each exosome carries a molecule signature distinct to the type of cell that spawned it. To selectively isolate just the exosomes from neurons or from oligodendrocytes, the researchers had to find an antibody that would specifically bind to a molecule only found on the desired type of exosome. This was challenging and delicate work, for which Suman Dutta, the paper’s first author, drew on his extensive expertise in working with exosomes. “The blood sample processing is complex and crucial and still has room for improvements,” Dutta said. “There are a lot of little details that can go wrong,” added Bitan.
Another unique feature of the project was the study population that the researchers worked with to develop the test. Rather than selecting a uniform population who all had textbook cases of Parkinson’s, Bitan and his colleagues evaluated the test in a broader group of patients. “Because in the clinic you’re going to get all kinds of people with all kinds of levels of diagnostic certainty, with different types of comorbidities – we thought, let’s try this,” Bitan says. “Let’s let them all in and see how objective the biomarker is.”
For the moment, Bitan emphasizes that the test is only appropriate for research purposes, and is not yet available for diagnosing patients. “The next steps are to do validation work in larger cohorts before it can become available to the general public,” he says.
Learn more about the Movement Disorders program at UCLA Neurology.
Caroline Seydel is the author of this article.