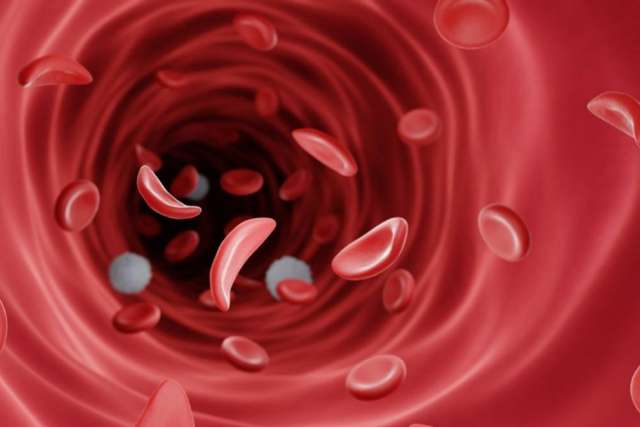
Photo: With sickle cell disease, red blood cells become stiff and sticky and take on a crescent shape, in contrast to the normal smooth, disc-shaped cells.
A new center at UCLA Health is striving to improve quality of care and increase life expectancies for patients with sickle cell disease.
In addition to primary and preventive care, and early management for complications, the comprehensive center of excellence is providing access to specialty care that often is lacking for patients with sickle cell disease.
“We live in a city that has significant health care disparities, and this is exemplified by sickle cell disease, which primarily affects people of color,” said E. Dale Abel, MD, PhD, chair of the Department of Medicine in the David Geffen School of Medicine at UCLA and executive medical director of the UCLA Health Department of Medicine. “The care of people with sickle cell disease has been spotty, at best, and very fragmented.”
Debilitating symptoms
Sickle cell disease is the most common genetic disease in the U.S. It predominantly affects African Americans, along with a smaller number of Latinos and other ethnic groups.
In people with sickle cell disease, red blood cells, which normally are disc-shaped and smooth, become stiff and sticky and develop the shape of a crescent. Because the cells survive only days, rather than for months, people with the disease are prone to anemia, with symptoms including fatigue, dizziness and shortness of breath. They’re also vulnerable to stroke, vision loss, lung troubles and infections.
The misshapen cells often clump together, blocking small blood vessels. These snags cause agonizing episodes centered on the limbs, back or chest. The reduction of blood flow can damage bones, skin and vital organs.
“There’s hardly an organ system that’s not affected by the sickle process,” said Gary J. Schiller, MD, a hematologist and director of the Bone Marrow/Stem Cell Transplant Program.
Barriers to care
As Dr. Abel noted, access to appropriate health care resources is a significant problem for patients with sickle cell disease, an assertion that is supported by organizations such as the CDC Foundation, an independent nonprofit that works closely with the Centers for Disease Control and Prevention.

The foundation reports there are a limited number of physicians who are trained and willing to treat adult patients with sickle cell disease. And because most patients with sickle cell disease are covered by Medicaid rather than private insurance, fewer doctors accept their government insurance.
In addition, people with sickle cell disease may be inaccurately perceived as drug seekers, and they often face longer waits to see a doctor or receive pain medication when visiting an emergency department, according to the foundation.
Disparities are also reflected in shorter life spans. Nationwide, the average life expectancy for a person with sickle cell disease is about 60 years. In California, it is 43 years for women and 41 years for men, Dr. Schiller said.
Additionally, Californians with sickle cell disease have higher rates of emergency department visits and hospitalizations than those in other states.
“We don’t do a good job of taking care of patients with sickle cell in California,” Dr. Schiller said. “We don’t really have adult-focused programs.”
Dr. Abel said he is hopeful that UCLA Health will be able to improve lifespans through accessible, high-quality primary care. It has been clearly demonstrated that disease-specific centers such as the new UCLA Health sickle cell disease center can reduce complications, emergency department visits and hospitalizations.
“Anything that has to be built literally from the ground up will take some time to affect all of the lives that need to be touched,” he said. “It will probably take a number of years for us to really turn around the statistics in this community, but it is worth every bit of effort and every penny of investment we are putting into this.”
Statewide effort
An estimated 100,000 Americans have sickle cell disease, with about 9,000 in California. Los Angeles County has the largest number of people with sickle cell disease in the state.
“There’s probably about 2,500 adults with sickle cell disease in L.A. County, and most of them do not have primary care or access to a hematologist,” said Alice Kuo, MD, PhD, who is working with Dr. Schiller to launch the center.
Dr. Kuo, a professor of internal medicine and pediatrics, said patients with sickle cell disease will be seen for primary care needs in Redondo Beach, Santa Clarita and downtown Los Angeles. The physicians treating them will undergo specialized training.
Patients will be able to receive fluid hydration, pain management, social support and other care seven days a week, Dr. Schiller said. Intravenous fluids to prevent dehydration can stop the sickling process and prevent severe pain that can lead to emergency department visits. Patients also will have access to clinical trials, which include medications for treatment and gene editing that has potential to offer a cure for sickle cell disease in the coming years.
“The new program attempts to create the same kind of comprehensive center that exists for hemophilia or cystic fibrosis,” Dr. Schiller said. “These kinds of centers in the community have been shown to significantly decrease emergency room visits, hospitalizations and length of stay.”
Patients also will have quarterly telehealth visits with hematologists based in Westwood. It is expected that only a fraction of patients will require more complex care or hospitalization.
UCLA Health is hiring a dedicated patient-services representative to help new patients navigate the system. Patient referrals to the new center will come from NCSCC case workers.
Dr. Kuo said she is hopeful that, in the coming years, UCLA will be caring for most adults with sickle cell disease in the region.
“My goal is not just to increase the life expectancy of patients, but also to increase their quality of life,” Dr. Kuo said. “I hope that by giving them access to high-quality primary care, we will take care of their medical condition and get them on the right path to learning how to manage their condition, so they can then live their lives to the fullest.”
The center is open from 8 am to 5 pm, Monday through Friday; for an appointment, call 310-267-1654.
Courtney Perkes is the author of this article.