An estimated 3 million people in the United States are living with recurring, unprovoked seizures that often affect their ability to live normal, independent lives.
Though there are more than 30 antiseizure drugs on the market, roughly a third of people with epilepsy have seizures that can’t be controlled by medication. Surgically removing part of the brain can be curative, but only for a small subset of individuals. For those with drug-resistant epilepsy for which resective surgery is not a possibility, seizures might be a monthly, weekly, or even daily experience.
But there is another option.
At UCLA Health, specialists can offer patients three kinds of neurostimulation, which send electrical signals to the brain through battery-powered, implanted devices: responsive neurostimulation (RNS), vagal nerve stimulation (VNS) and deep brain stimulation (DBS).
The devices’ electrical currents affect the excitability of brain circuits, which can reduce the frequency of seizures or, in some cases, prevent them altogether.
“Beyond the effects on quality of life, patients with drug-resistant epilepsy have a high risk of sudden unexplained death,” says Dawn Eliashiv, MD, a professor of neurology in the David Geffen School of Medicine and co-director of the UCLA Seizure Disorders Center. “All three of these neurostimulation modalities have shown effectiveness in reducing that risk.”
Three methods of therapy
Receiving any type of the three neurostimulation methods begins with a minimally invasive procedure in which a device is implanted into the patient’s body, though each therapy targets a different stimulation pathway.
Vagal nerve stimulation is the oldest form of neurostimulation, with the first device implanted in the United States in 1988 and receiving FDA approval in 1997. The VNS device is implanted under the skin on the left side of the chest and connected to a wire that is wrapped around a vagus nerve in the neck. Electrical stimulation travels from the nerve to certain areas of the brain, altering neural activity.
Though the therapy is still available today and could be the best option for some patients, there are other neurostimulators that may be more effective. Specialists at UCLA’s Seizure Disorder Center carefully review each patient case to decide which type of neurostimulator would work best.
For deep brain stimulation, a surgeon implants the device under the skin in the patient’s chest or stomach, and an electrode is run into the thalamus — a critical part of the brain that has extensive connections to other neural regions and plays a role in sensation, movement and cognition.
Both VNS and DBS have their limitations, Dr. Eliashiv says. Primarily, the stimulation for both kinds of devices is delivered on a preset cycle, rather than in a response to a seizure.
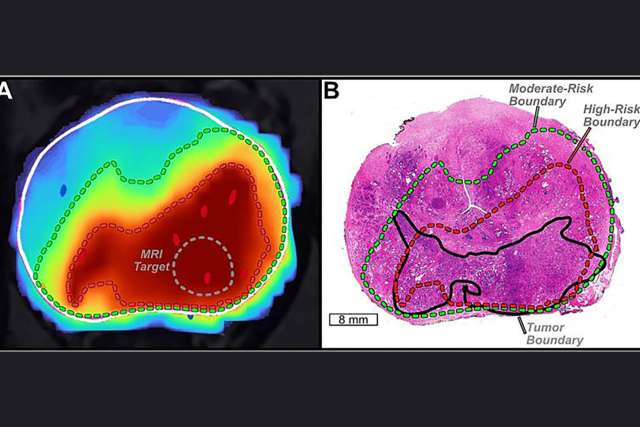
Responsive neurostimulation overcomes this constraint as a unique closed-loop, brain-responsive system. Rather than sending continuous, pre-set stimulation to the brain, the device is specially programmed to detect seizures and deliver a small amount of electrical current when one is coming on.
The device also allows doctors to continuously monitor the frequency, timing and location of electrographic activity. Each patient is given a remote monitor, which they hold over their implanted device at least once per day. The patient then uploads the data stored on the monitoring wand to a secure website, where their medical care team can review brain activity and make adjustments.
“Now that we know how to program better, we are seeing patients achieve really remarkable results,” Dr. Eliashiv says. “The benefit of the therapy is that it really is personalized for each individual’s seizure fingerprint.”
Results and effectiveness
In a real-world retrospective study of 150 patients who received RNS, nearly 80 percent had their seizures cut in half after two years of use, and 1 out of 3 reported periods of no seizures for six months in a row.
Beyond the therapy’s effectiveness in reducing seizures, the RNS device is able to capture a wealth of real-time information, which is providing researchers with deeper insights into how to treat epilepsy and other neurological conditions.
As the principal investigator on the post-approval study of RNS and DBS, Dr. Dr. Eliashiv is monitoring the long-term effects of the therapy. She is also working with collaborators throughout UCLA Health to investigate other questions, such as why certain patients might be resistant to medication and which type of neurostimulation would be most effective for each individual patient.
“Since we have the device, we’re able to do interesting, real-time experimental trials looking into brain function,” Dr. Eliashiv says. “We now have a window, which was previously unavailable with other devices over the years, to monitor intracranial brain activity.”