For everyone delivering care to COVID-19 patients in UCLA Health System’s ICUs, the pandemic has been a dark and tumultuous time, but also one that has been brightened by surprising flashes of light and hope.
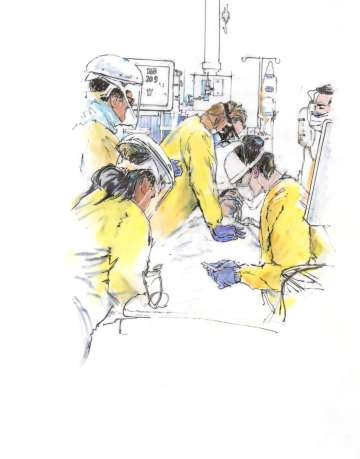
Since the COVID-19 pandemic began to really hit home, in March 2020, the doctors, nurses, respiratory therapists, care partners and others working in the medical ICUs of UCLA and its affiliated hospitals have been on the frontline of providing ongoing care to patients critically ill from the disease. They have performed dangerous intubations, placed essential lines, done CPR when nec - essary, held a cell phone to the ear of a crit - ically ill husband, wife, parent or sibling to hear the voice of a loved one and, too often, been the only ones present in someone’s final moments. Here, in their own words, drawn from emails, social-media posts and journal entries, are reflections and experi - ences from some of this team of heroes.
I still remember like it was yesterday, pressing on the kid’s chest. I say kid because he wasn’t even 30 yet. I didn’t even have time to throw on the PAPR, knowing that compressions would aerosolize the disease. I looked at my colleagues who feared entering the room because of that. A couple of nurses quickly threw on PPE and took a chance and came into the room to help. It was a very intense moment. I just couldn’t bear the thought of COVID taking a life of someone so young, and I couldn’t stop caring, even though my own life was at risk.”
— Romain Penet, RN
“This is our moment; we have been called. And though we may have been drafted into a ‘war’ none of us saw coming, we are ready to step up to help our community. I have taken a lot of inspiration from others who have highlighted the unique privilege we have in this crisis to be capable of helping. And that is a calling that will help me to push through any of the fear or doubt, knowing we, together, will pull through this.”
— Lawrence N. Benjamin, MD, first-year pulmonary/critical care fellow
“I have always thought the 4ICU was a special place, where we see all kinds of deterioration and unstable patients, but witnessing such a high degree of professionalism on top of such camara - derie throughout this pandemic has changed my nursing practice forever.”
— Catherine Fairbanks, RN
“I just left the hospital after a 14-hour day, walked back to my hotel room, and I think I need a long, good cry tonight. I cry for the patient I just lost. I cry for the mother who is not allowed to be at the bedside of her disabled son. I cry for the patient who hasn’t seen her husband for nearly three months. I cry for the newly widowed husband. I cry for the protestors. I cry for the senseless loss of Black lives. I cry that there is a need for curfews and military in the city I love. I cry for the businesses that have been looted and de - stroyed. I think of all the reasons we have to cry right now, and I cry harder.”
— Thanh H. Neville, MD ‘05 (RES ‘08, FEL ‘11), attending physician

“There was a moment at the beginning of the COVID crisis when my heart sank. I was in charge of our UCLA Health System ventilators and found myself surveying both my thoughts on our hospital’s current inventory state and what that potentially looked like against the worst-hit hospitals across the country. It was like standing at the foot of Mt. Everest, staring up and consid - ering the massive terrain and elements. Where do I start the task? Eventually, you realize that your lamp may not shed enough light for you to see what’s in the far distance, but it will illuminate the path that’s right in front of you. If you take one step at a time, you find yourself making the necessary progress to become successful.”
— D’Mitri Champion, clinical operations manager for Respiratory Therapy Services
“There has been a lot of talk about ‘resilience’ among health care workers. I am not a fan of this term. Resilience is defined as an ability to recover from or adjust easily to misfortune or change. ‘Grit’ is a better word. Grit is showing up every day, no matter how hard it is, or how tired you are, or how scared you are. It is putting on PPE when the skin on your face is bruised and broken. It is adding on an extra shift because we are desperately short on staffing. Grit is showing compassion when you have nothing left to give. It is smiling when it seems like there is nothing to smile about. Grit encompasses passion and perseverance. I’m not sure that any of us have recovered from our experiences over this past year. And when we do, we will never be the same. But we have grit, and we will persevere.”
— Nicole Agee, RN

“Most days, if I squint, I can see some silver lining in this new world — which can be described as some sort of wonderful combo of kind - ness, gratitude, support, resilience, generosity, strength and solidarity. And even some hope that many lives can be saved and that maybe we will become better humans and physicians in the process.”
— Tisha Wang, MD (RES ‘05, FEL ‘08), pulmonary/critical care clinical chief
“I’ve seen some amazing stories of survival, many patients on the brink of death who pulled through with our help and who are now at home safe with their families. I’ve seen just as many heartbreaking stories of defeat, including a patient who promised to give me golf lessons if I got him through COVID. Sadly, those lessons will have to wait until we are both reunited on the golf course in the sky.”
—Jaime Betancourt, MD, attending physician
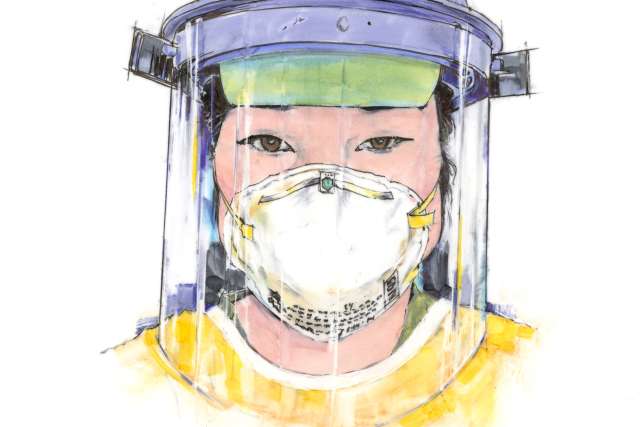
“Truly being present, bearing witness and providing the care and comfort at these COVID-19 patients’ most vulnerable and scared time is the essence and the heartbeat of nursing. With misty eyes, we are together in this.”
— Sherry Xu, RN, unit director
“Walking into the rooms of our first COVID-19- positive patients was extremely nerve-racking, but knowing we all felt the same was something of a comfort to everyone involved in their care. Assisting with the organization and training of the emergency-response team was one of the most rewarding things I have done in my career. This experience has shown what we all are capable of, and for that I am forever grateful.”
— Matthew Dartt, assistant director of Respiratory Care Services
“First, there was fear. Would the PPE actually protect us? How do you best treat a novel virus? Then, there was community. The nurse would help me don my PPE, and I would check the patient’s urine output inside the room to minimize the nurse’s exposure. Outside of the hospital, it was social isolation, yet inside the hospital, I felt more connected than ever. Now, there is grief. Too many patients are dying. Those who survive are seen in our post-ICU clinic with a tremendous road to recovery ahead. So we continue onwards, both for them and for us, and we put our heads together and work.”
— Kristin E. Schwab, MD (RES ‘16, FEL ‘20), co-director of post-ICU recovery

“I began my training in the MICU during COVID-19. I was assigned COVID-19 patients for one full month. Needless to say, I learned more about respiratory distress, PPE and ventilator management in one month than I did working the one year since I was hired.”
— Ferdinand Castro, RT
“This ICU week is particularly horrible. During my last stint, I had discharged the last COVID patient, but this week, there seems to be a new patient transferred to the ICU with COVID every day. Today, we admitted the patriarch of a family, all of whom have COVID. He wants his daughter to have his durable power of attorney. My residents tell me all she does is cry on the phone; I cannot bear to call her myself. We asked the patient to enroll in a clinical trial, and he consents, stating, ‘Even if I don’t benefit from this study, I hope the infor - mation will help others.’ I am so tired of kindness being a poor prognostic factor.”
— Thanh H. Neville, MD ‘05 (RES ‘08, FEL ‘11), attending physician
“While I’ve been fortunate enough to take care of many kind, amazing patients, I don’t think I’ve ever heard as many words of gratitude and appreciation as I did last week. Although these #CovidWarriors were essentially recovering from near-death experiences, they still asked how they could help others, by donating plasma or offering sup - port to people who have survived the same or by doing something else positive. They cared about things bigger than themselves.”
— Nida Qadir, MD, attending physician
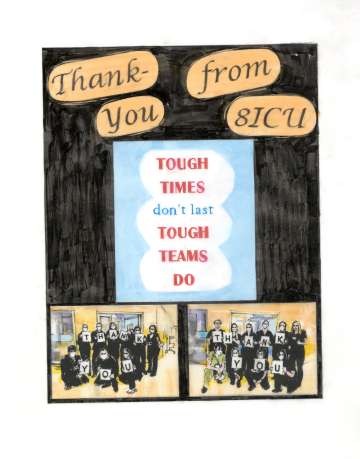
“Work has been a mentally and physically challenging time with magnified emotions. We’ve seen both unexpected recoveries and unfortunate losses. Given the circumstances, we’ve found our own ways to celebrate life, whether that be through lining up to clap for a patient being discharged or providing our patients a personal experience through our 3 Wishes Program as they transition on. The teamwork among all the staff — doctors, nurses, therapists, care partners — shows how resilient we all are.”
— David Yadao, RN
“I recall a gentleman struck hard by COVID that landed him in the ICU. Even though he was alone, we assured him that he wasn’t. I felt the highs and lows of this patient case. To see him get reintu - bated numerous times, I was almost losing hope. I did my best to keep him connected to his wife via video chats, and when I overheard how much he meant to his family, I could no longer think negatively. The doctors, nurses, care partners and ancillary staff did a magnificent job of staying calm and patient throughout his course. He beat COVID and was reunited with his family. It was such an awesome moment.”
— Luis Sandoval, RN
During these dark days, I received an email from the wife of a successfully discharged post-ICU COVID-19 patient. She is giving me words of encouragement and writes, ‘We are forever grateful. This is nothing compared to giving us life. Giving our kids a father. Helping me not be a widow. Please focus on all the people you save. We are some of them.’ She included a picture of her husband writing me a thank you card. This is a man I put an endotracheal tube down! Needless to say, I cried.”
— Thanh H. Neville, MD ‘05 (RES ‘08, FEL ‘11), attending physician
“I’m coming to appreciate that I get to witness such a dramatic range of human experiences and emotions in the work that I do. I can either be drained by this reality or I can embrace the possibility that it may give me wisdom that I otherwise would not have obtained.”
— Nida Qadir, MD, attending physician
“Anxiety is pretty high right now at the hospital, between how difficult it is to predict how patients will do, how to counsel patients and their families, and the worry about the well-being of colleagues. I can only imagine what it’s like for those nurses, the other fellows, the RTs or attendings who have families at home and some of the decisions being made about whether to re - move themselves from their loved ones or simply return home and take as many precautions as they can. I have the ability to essentially quarantine myself at home after work, so I don’t risk infecting others, though it has been pretty isolating. My parents are worried sick, but I’m reassuring them as much as I can.”
— Lawrence N. Benjamin, MD, first-year pulmonary/critical care fellow
I checked in on a trainee of mine last night who is quarantined. Made sure they were doing ok. Got a reply that they were fine but frustrated about being ‘put on the bench.’ That made me smile for the first time yesterday. It is the ‘put-me-in-coach’ attitude, even when you are potentially walking into a fire, that makes me love and appreciate the people that I am surrounded by.”
— Tisha Wang, MD (RES ‘05, FEL ‘08), pulmonary/critical care clinical chief
“I’m sleep deprived, physically tired, mentally exhausted and about as beat up as I’ve ever been after an ICU rotation, but I’m happy and proud of the work my team and I did, and continue to do, every day.”
—Jaime Betancourt, MD, attending physician
“I am so very thankful to work alongside a compassionate and hardworking team in the MICU and all ICUs. Not only do we support each other and help each other out to meet the needs of our patients, we are all there for each other emotionally as well.”
— Amanda Hill, RT
“The hardest thing every day is to have to bet against your fears of a dreaded outcome, to pray that the inert patient in the bed is not suffering, to hope that their family will see them again, to bat away fears of futility and the memories of the times you’ve withdrawn pa - tients from care. It is a struggle to consciously expend energy to undermine the validity of your instincts and experience, all in the name of hope.”
— Kimberly Coppin, RN
“As I sit here thinking of my mom’s battle with COVID, it’s hard not to question every decision made along the way. I think of all that was done and how things could have been different. I think, ‘What if I would have brought her to the hospital earlier? What if she would have received remdesivir? What if we didn’t intubate her on May 12th and had waited?’ I’d have one more day with her. I could tell her how much she means to me and how much I love her without feeling rushed. I could have let her know I couldn’t have asked for a better mother. I could have talked to her about what she wanted done if she reached a point where her quality of life did not meet her standards. But, oh, how she wanted to live! She could have told me what dress, shoes and jewelry she wanted to wear as she was laid to rest. She could have told me who she wanted to receive her jewelry, clothes, furniture, etc. She could have told me what bills needed to get paid. But, then again, we never thought she was going to die.”
— Cindy Valadez, RN
For my entire career, if I ever intubated someone for what I believed could be the last time, I invited their loved ones into the room while I prepped and encouraged both parties to say to each other anything they wanted to say. I could write a book about the final words I have heard, often fighting back my own tears. Being present in those moments is hard in its own way, but now, often it’s just the docs and the patient, and so many of these patients are terrified, crying and often asking the health care professionals in their final moments to not let them die. Now we are the only ones who might hear their last words.”
— Tisha Wang, MD (RES ‘05, FEL ‘08), pulmonary/critical care clinical chief
“There I was, making out my will, preparing to die, nauseated, scared and in scrubs going to work in the COVID unit. It is not what you think. Well, yes, it was, and is, a war zone. But in the war zone was LIVING, BREATHING TEAMWORK, GENER - OSITY OF KNOWLEDGE, CARING, CHEERING WHEN A PATIENT MADE IT, YELLING WHEN A NURSE WENT IN A ROOM WITH NO PROTECTION TO PREVENT A PATIENT FROM EXTUBATING THEMSELF. I was witnessing and experiencing a type of nursing like no other. Everyone trained me. I loved working in MICU. We were doing everything together as a team. The more we learned about COVID, the more we became the warriors against it.”
— Meilani Renger, RN
“I’ve gained an even deeper admiration and respect for my nurses and respiratory therapists, the true frontline heroes in this COVID nightmare we are living. My ability to help any patient is only as good as those who execute my orders, and I am thankful I work with so many like-minded heroes and heroines.”
— Jaime Betancourt, MD, attending physician
“We trached a man despite his COVID PCR continuing to be positive, because we didn’t think this represented true infection. But, truth be told, even if it was abso - lutely clear he was positive, I would still have done the trach, because I wanted so badly to give him a shot. He went home after a long hospitalization, and he was doing well. Then I heard he had a sudden cardiac arrest. It’s been story after story like this for months. These stories have taken a piece of my soul that I don’t think I’ll ever get back. Like many of us, I’m certain I’m going to emerge a different person when this is all said and done, hopefully for the better, but who knows.”
— Nathan Yee, MD, third-year pulmonary/critical care fellow
“Our souls may never be the same.”
— Tisha Wang, MD (RES ‘05, FEL ‘08), pulmonary/critical care clinical chief