Marcus A. Horwitz, MD, knew he would be an outlier. It was March 2020, COVID-19 had exploded and everybody was frightened and frantic to stop it. A vaccine was one answer, and therapeutics was another. Long before Pfizer and Moderna would make headlines with their vaccines, multiple pharmaceutical companies and universities in the United States and around the world were steaming ahead with their own research. In the race for a vaccine, some 200 potential candidates were in the works. Some were yet just a gleam in a scientist’s eye, others were further along. Dr. Horwitz wanted in.
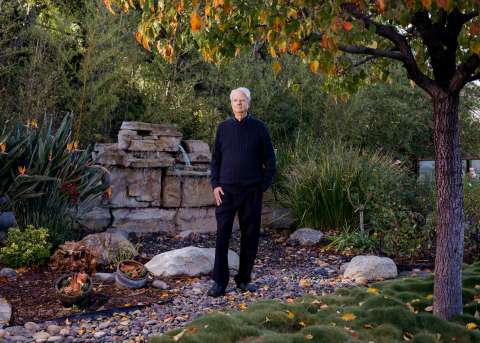
Dr. Horwitz is a Distinguished Professor of Medicine, Microbiology, Immunology and Molecular Genetics in the David Geffen School of Medicine at UCLA. He was not a COVID-19 expert, but for 35 years he has been building and perfecting vaccines against Tier 1 agents of bioterrorism — anthrax, tularemia, plague and the like — that cause respiratory infections and can be lethal. He also was instrumental in developing a vaccine against tuberculosis, which is spread through coughs and sneezes and kills some 1.4 million people worldwide every year.

So it wasn’t hubris that Dr. Horwitz was bringing to the table; it was expertise. “We were late to the game, but we thought we might have something that could help,” he says. “Even though we hadn’t worked with viruses before, we felt we might be able to make a contribution.”
Still, there were hurdles. First, his comment that “we hadn’t worked with viruses before” could easily have been a non-starter. Dr. Horwitz is an expert in bacterial diseases; SARS-CoV-2 is a virus that causes the disease COVID-19. Second, they had no money. As an academic laboratory, Dr. Horwitz and his team were not eligible to apply for funding from Operation Warp Speed, which had been initiated by the administration of President Donald Trump to cover the huge costs of research and development to turbocharge development of a COVID-19 vaccine.
And, again, they already were way behind. So the question then became, why bother?
There were several reasons. What if other efforts didn’t pan out? What if they work but their efficacy plunges after a few months? What if the SARS-CoV-2 virus substantially mutates? And what of the cost and time delay in producing the millions of vaccine vials needed, and delivering them efficiently?
For all of these reasons, as Dr. Horwitz walked across a locked-down UCLA campus to his lab on a March morning, he decided to take a shot. Sitting down with Qingmei Jia, PhD, a project scientist in his lab, they devised a plan and got to work. A jump-start came in the form of a $50,000 grant from the UCLA AIDS Institute and its Charity Trek fundraiser, and, later, with permission from the National Institutes of Health, he and his team were able to use some money from one of their existing NIH grants.
DR. HORWITZ DID HAVE ONE BIG ADVANTAGE: He already had a solid vaccine “platform” with which to work. Over the course of his long career — Dr. Horwitz began his academic career at The Rockefeller University in 1980 and joined the UCLA faculty in 1985 — he had developed and refined a workhouse vector. A vector is the mail truck of biology, delivering antigens, a bit of the bacterium or virus that causes the particular disease you’re hoping to prevent, to provoke — hopefully — a response from the immune system. Using a harmless bacterium or virus as a vector to deliver antigens is one type of vaccine. Dr. Horwitz and his colleagues had created vaccines to protect against several bioterrorism agents, including tularemia, plague, melioidosis and anthrax. That work is ongoing.

Even though his vector was bacterial, he believed it could be modified for COVID-19. But building a vaccine is not an easy process. Scientists know that using a living organism as a vector to deliver a vaccine packs the biggest wallop. “When you inject a live organism into a body,” Dr. Horwitz says, “it basically sends out a lot of danger signals that tell the body to pay attention,” prodding the immune system to respond.
But it’s tricky, because one doesn’t want an organism that is going to harm the host. The scientists must design a vector that will give the immune system a kick in the pants to get its attention, but not cause harm.
In creating his original suite of vaccines, Dr. Horwitz used an organism that in the wild causes a less severe form of tularemia than the one caused by the closely related bioterrorism agent. (Tularemia is an infectious disease that attacks the skin, eyes, lymph nodes and lungs.) “So we started out with a strain of bacterium which is less virulent to begin with,” he says. They took a vaccine that utilized the same organism, called Live Vaccine Strain, or LVS, that was developed by other researchers decades earlier and had been used to deliver millions of doses, but it proved to be too virulent for Dr. Horwitz’s taste. “When given as a vaccine, it could give you a nasty infection,” he says
To improve the LVS vaccine and make it safer, they searched for and knocked out — deleted — a gene they thought rendered the vaccine harmful. It was not an easy task. Dr. Horwitz refers to it as the search for the “Goldilocks gene.” Like Goldilocks, whose first bowl of porridge was too hot (ouch), the second too cool (blah) and the third just right (yum), “It’s very easy to knock out some gene that’s going to make the organism so harmless it won’t arouse the immune system,” he says. “And it’s very easy to knock out a gene that doesn’t do much of anything to reduce the virulence of the organism. So, to get just the right one takes a little bit of experimentation,” he says.
Eventually, they found it — a major gene called capB. This made their modified vaccine, now called LVS ΔcapB, more than 10,000 times less harmful than the original vaccine tested in mice, yet it retained its ability to induce a strong immune response.

The next step was to use this platform to express antigens for the most virulent strain of tularemia, and it worked; the stronger immune response would now allow the vaccinated host to repel the highly virulent foreign invaders if it ever encountered them in the future. In subsequent work over the years, the researchers used this same strategy to develop vaccines against each of the other Tier 1 bioterrorism agents.
Now, they have applied the same strategy to combatting SARS-CoV-2, the virus that causes COVID-19. So far, the results continue to be “very promising,” Dr. Horwitz says.
IN ALL, THE RESEARCHERS CREATED SIX VACCINES, expressing four different proteins, using their vector. One was the S protein, the now infamous spike protein, which rests on the surface of the coronavirus, and is what the majority of the other vaccine candidates are targeting. By the end of April, five of the six had failed, but with the last, Dr. Horwitz had a potential winner. It was not the S protein. “The one we had great results with was the vaccine targeting the M and N proteins of the coronavirus,” he says. “The M protein stands for the ‘membrane protein,’ and the N protein stands for the ‘nucleocapsid protein.’ The M proteins are at the surface of the virus, and N proteins are inside the virus surrounding its RNA.” The two proteins proved to alert the immune system in an animal model to provide protection.
Indeed, before clinical trials can take place, every new drug must be tested in animals to ensure its safety and efficacy. With the other COVID-19 vaccines, most, says Horwitz, were tested using the rhesus macaque monkey, which he thinks is not the best animal model to use; in fact, he calls it a “low bar.” “With COVID-19, the rhesus macaque does not get sick,” he notes. “It doesn’t even get a fever. So, it’s a model of asymptomatic infection or very mild disease.” That means the only thing they can measure in the macaque given SARS-CoV-2 is the amount of virus in the mouth, throat or lungs.
While it’s too early to say, Dr. Horwitz fears that some of the other vaccines might only protect against “COVID-19 lite.” He hopes that’s not the case but says, “I don’t want to make a vaccine to protect against mild disease. I want to protect people who are going to get severe disease.”
To test his vaccine, Dr. Horwitz used the golden Syrian hamster. “Hamsters get severe COVID-19 disease, so they show substantial weight loss and they get a lot of lung pathology,” he says. The results are very promising. The animals challenged with SARS-CoV-2 were highly protected by the vaccine from severe weight loss, and they had virtually no pathology in their lungs.

Two other aspects of Dr. Horwitz’s vaccine stand out, assuming, of course, it proves to work in humans. Millions of doses of a bacteria-based vaccine can be grown overnight in a simple broth, he says. That’s unlike a virus-based vaccine, which must be grown in host cells and then extensively purified. Producing a virus-based vaccine “is an expensive, time-consuming process, which is why it will take these companies six months to make 50 million or so doses,” Dr. Horwitz says. “I can make 50 million doses in my own lab overnight, because bacteria replicate that fast. Extensive purification isn’t needed,” he says. (The vaccines being developed by AstraZeneca and many other companies are viral-vectored vaccines, while still other companies are developing vaccines utilizing inactivated or attenuated forms of the virus that causes COVID-19. The Pfizer and Moderna vac - cines were developed on what is knowns as a messenger-RNA — mRNA — platform, and no virus is involved.)
For purposes of transporting to hospitals, clinics and local drugstores, another advantage is that a bacteria-based vaccine can be freeze-dried and kept viable as a powder, which then can be shipped at normal refrigerator tempera - tures. That eliminates the need for expensive sub-zero refrig - eration, as is necessary for the Pfizer vaccine, which must be stored at minus-94 degrees Fahrenheit.
Finally, Dr. Horwitz is optimistic his COVID-19 vaccine may provide protection for future SARS-related infections. That’s because viruses mutate. Dr. Horwitz notes there was a SARS epidemic in 2002-03 caused by SARS-CoV-1. Now we have SARS-CoV-2. “If you compare the proteins of SARS-CoV-1 and SARS-CoV-2, the spike protein, for example, is 76 percent identical. From the standpoint of biology, that’s a huge differ - ence,” he says. But if you look at the M and the N proteins, the ones Dr. Horwitz’s vaccine targets, they’re 90 percent identical — they’ve changed much less. “Because they’re so similar, our vaccine potentially could protect against a future SARS-CoV-3, in addition to the current SARS-CoV-2,” he says.
Now it is a waiting game. The next step would be to manufacture Dr. Horwitz’s vaccine and conduct human clinical trials. He has been in discussions about this with the National Institutes of Health. Time will tell which vaccine, or vaccines, will prove to be the magic bullet the world is hoping for.
IS IT SAFE, AND DOES IT WORK? THOSE ARE THE NEXT QUESTIONS to answer once construction of a vaccine is complete. For that, clinical trials are the gold standard. Conducting and completing a clinical trial for any drug is not an easy task. There are lots of trials, people lead busy lives and many are understandably nervous about putting a new drug into their bodies. This is particularly true among many Blacks and Latinos, whose communities have been hardest hit by COVID-19. In fact, in the U.S., only 32% of Black adults say they would definitely or probably take a COVID-19 vaccine, according to the Pew Research Center.
Dr. Jesse Clark, MD (FEL ’08), an infectious-diseases specialist and associate professor-in-residence in the UCLA Department of Medicine, is medical director of the UCLA Vine Street Clinic, in Hollywood, which was a site for the Moderna vaccine clinical trial last year.
“There’s a historical legacy of discriminatory treatment in people of color being used as sort of guinea pigs in a trial without actually reaping the benefits of a study,” Dr. Clark says. “Understandably, they are concerned.” Because COVID-19 hits Blacks and Latinos so hard, “we were particularly invested in working with these communities to make sure people of all ethnicities were involved in the trial.”
The clinic had a team that put out feelers and publicized the study in the local community and through social media, Dr. Clark says. There was a clinical trial network that had a national website where people can register. UCLA Health also set up a referral website on its main page.
“We really wanted to make an effort to reach communities and populations that are underrepresented in research,” says Chris Blades, community program manager for the Vine Street Clinic. “There has been such a heavy burden on them during this pandemic.”
While response from the community generally was good, many people still were anxious about participating in the trial, Blades says. “There was a bit of hand-holding, a bit of phone tag before setting up an appointment. There was confusion about the science and about what was being reported in the media, and so it was very important that the messages we were putting out were clear and consistent.”
Once that trust was established, the clinic worked with willing volunteers to reach out to others within their social network “to bring more people into the trial who look like them,” Blades says. That approach proved to be very fruitful. “Because someone they trust would vouch for us, they went out on a limb and joined,” he says. “I feel we were able to attract people that way who probably would not otherwise have participated in a study like this.”
Shawn Griffin didn’t need any encouragement to join the study. He is 58 years old and African American. “I had read about trials in general and that not enough people of color were involved,” he says. “Too many people don’t trust what’s going on.” But he wanted to be involved. “I don’t know anyone who’s been sick or died from COVID-19, but hearing people’s stories and having empathy for what they’re going through really encouraged me,” Griffin says. “With everything going on politically with people not trusting scientists, it makes me want to bang my head against a wall. Something’s got to happen. And if we all just sit around, nothing’s going to happen. I want to be a part of the something that happens.”
Griffin said he also is honoring the memory of his mother, a nurse who died in 2020 from causes unrelated to the pandemic. “She taught me that you’ve got to do stuff for the greater good, even if sometimes the greater good doesn’t understand you,” he says. To those who tell him he shouldn’t participate in the trial, “I tell them I am happy with my decision. I feel good about my decision.”
EVEN AS THE BIG PHARMACEUTICAL COMPANIES WERE GETTING READY TO ROLL OUT THEIR VACCINES and a national inoculation program was to begin, some lawmakers continued to advocate for letting the virus run its course in the hopes of achieving what is called “community immunity,” or “herd immunity,” which is when enough people have become immune to an infectious disease, either through being infected themselves or having been vaccinated, that the virus has no place left to spread and fades away.
But taking such a course would come at a terrible cost. “We are not in the middle of a second or third COVID-19 wave; we’re in the midst of a COVID-19 tsunami,” says Robert J. Kim-Farley, MD, MPH, professor-in-residence in the UCLA Fielding School of Public Health and former director of the Division of Communicable Disease Control and Prevention at the Los Angeles County Department of Public Health. In such a scenario, up to 2 million Americans would die before the country reaches community immunity, he says. That’s too high a price to pay, and Dr. Kim-Farley believes the virus itself will help us achieve community immunity by encouraging more people to accept taking a vaccine. “This tsunami of cases will have people reevaluating their opinion about vaccines, and they will be more inclined to take it as they see more people they know become sick and, perhaps, die,” he says.
But given the cynicism about Big Pharma — a 2019 Gallup Poll found that Americans rank the pharmaceutical industry last for confidence among 25 industries that Gallup evaluates — people have concerns about manufacturers cutting corners to speed up the process. They are concerned about political pressure, too, the “warp speed” to develop a vaccine quickly.
That level of unease, too, should abate as vaccines show themselves to be efficacious and safe. “People will get more comfortable with receiving COVID-19 vaccines as they see the FDA and independent medical boards reviewing all these data, ensuring these vaccines have high efficacy and a strong safety profile,” Dr. Kim-Farley says. He also notes it is not in pharma’s self-interest to cut corners. “Can you imagine the public relations disaster if one of these companies were caught falsifying data?
Finally, he anticipates a rolling wave of public health messaging that encourages vaccination and addresses any remaining concerns that people may have as the vaccination program gains speed.
It eventually will be clear how effective the current vaccines — and possibly outliers like the one developed by Dr. Horwitz — will be. But it remains everyone’s hope that an end to the pandemic will come soon. Says Griffin, the clinical trial participant, “It breaks my heart on both ends of the spectrum — the older people who have died alone, isolated in an ICU, without having a chance to say goodbye to their loved ones in person, and the younger people who are losing their moment in time and having to put their lives on hold. “I just want for all of us to get back to the life that we knew before."
