The COVID-19 pandemic has laid bare the realities of long-standing racial inequities in the American health care system, conditions that are exacerbated by the deep seams of disparities that cut through every layer of society and now are the focus of the movement to address racial injustice.
“Poverty and racism lead to unfavorable housing conditions, high-risk employment and poor access to care,” says Folasade May, MD (FEL ’15), PhD, a health-equity researcher and quality director at UCLA Health and director of UCLA’s Melvin and Bren Simon Gastroenterology Quality Improvement Program. “All of these circumstances put Black and Latinx people at greater risk of contracting and dying from COVID-19.”
While the media’s portrayal of COVID-19 implies that Blacks and Latinos, because of their poor health status, will get the virus and die, “little attention is focused on the role of labor practices in which Blacks [and Latinos] in America work in occupations and places that are more likely to put them at risk of being infected,” says Vickie M. Mays, PhD, director of the UCLA Center on Bridging Research Innovation, Training and Education for Minority Health Disparities Solutions.
“Rarely do we hear about the numbers of Black [and Latino] Americans who work in essential jobs” — as bus drivers, hospital custodial staff, meat packers, aides in nursing homes, and the like — “often with no sick days or ability to work from home,” Dr. Mays said in an article in UCLA Public Health magazine, the publication of UCLA’s Fielding School of Public Health, where she is a professor of health policy and management. “Black [and Latino] Americans are at high risk for COVID-19 based not just on their health disparities, but also on disparities that exist based on a lack of health care resources, the ability to respond to stay-at-home orders, effective isolating at home because of the lack of space in their living quarters, or a lack of income that allows them to purchase goods only for a few days at a time, requiring more store visits.”
The observations by Drs. May and Mays are borne out in the numbers. According to the Centers for Disease Control and Prevention, among the more than 28 million Americans who have, as of February, tested positive for COVID-19, hospitalization rates have been five times higher for Blacks and four times higher for Latinos compared to whites. Patients who have other pre-existing conditions, such as diabetes, obesity or cancer — particularly those of color — have suffered higher death rates and longer hospitalizations, according to several studies.
It is not just physical health that is at issue. “The disparities in mental health care in communities of color are tremendous,” says Gail E. Wyatt, PhD, professor of psychiatry and biobehavioral sciences in the UCLA Semel Institute for Neuroscience and Human Behavior and director of the Center for Culture, Trauma and Mental Health Disparities. “Services to these communities are inadequate, and the rate of suicide is increasing without appropriate resources for treatment. When problems are noted, they often are criminal - ized rather than treated. This is a glaring historic gap in our health care system; it has been a focus of my work for more than four decades,” she says.
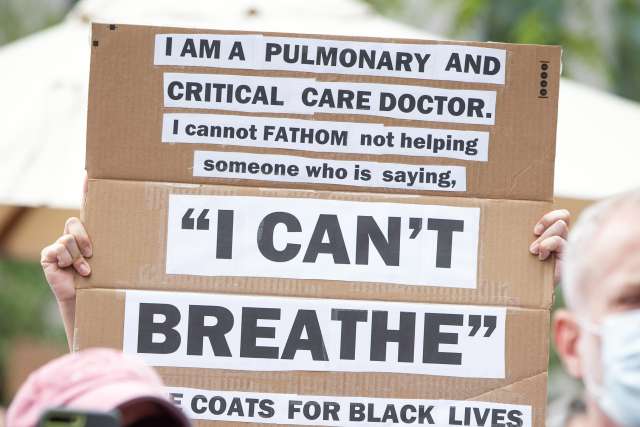
THE CONFLUENCE OF THE PANDEMIC AND THE BLACK LIVES MATTER MOVEMENT that grew in 2020 in the wake of the killings of George Floyd, Breonna Taylor, Ahmaud Arbery and many others over the past years has caused health care systems across the country to take a deep inward look at how they have addressed issues of racial disparities within their institutions and the communities that they serve. Within the UCLA Health System and the David Geffen School of Medicine at UCLA, the events of 2020 created a sense of urgency and a call for action to do more, and to do better when it comes to diversity, health equity and inclusion
The events of this past year “have caused sorrow, confusion, anger and frustration for all of us within the UCLA Health community and throughout the country and the world,” says John C. Mazziotta, MD (RES ’81, FEL ’83), PhD, CEO of UCLA Health and vice chancellor for UCLA Health Sciences. “The senseless killings of George Floyd, Breonna Taylor and many other unarmed African Americans, as well as the subsequent Black Lives Matter protests, demonstrate the pain that our country has continued to endure sec - ondary to systemic racism. The health and social injustices that we have witnessed are intolerable to everyone, especially to those of us in health sciences, and they must be eliminated.”
As one of its first steps, UCLA Health took a lead among academic medical centers in advancing major initiatives, both in its school of medicine and hospital and clinic system. The UCLA Hospital and Clinics System created an executive position — chief of health equity, diversity and inclusion — to advance change throughout the UCLA hospitals and clinics. The David Geffen School of Medicine at UCLA took steps to amplify the work of its Office of Equity and Diversity Inclusion, led by Lynn Gordon, MD (RES ’88, FEL ’89), PhD, senior associate dean for equity, diversity and inclusion, and created an ambitious initiative, the Anti-Racism Roadmap
The scope of the chief of health equity, diver - sity and inclusion position cuts across all areas of the health system enterprise. “In addition to equity, diversity and inclusion in our workforce, and in everything that we do, this position really is about how we build in that health-equity piece to make sure that we are doing everything we can to remove barriers to access to care and to address any health disparities that we are seeing,” says Johnese Spisso, MPA, president of UCLA Health and CEO of UCLA Hospital System.
Medell K. Briggs-Malonson, MD (RES ’09, FEL ’12), MPH, associate professor of emergency medicine and chair of the UCLA Department of Emergency Medicine Equity, Diversity and Inclusion Committee, was appointed in September as interim chief. “This is an important and exciting movement within our system, and we are developing it in a way that is optimistic, that is hopeful and that is grounded in unity and bringing us all together,” Dr. Briggs-Malonson says. “We know that there are significant issues that we need to address, and we are going to do it in a way that visualizes how we as UCLA Health want to be three years from now, five years from now, 10 years from now. How are we going to support one another as colleagues? How are we going to make sure that we provide the best care to our patients, regardless of their identities? That’s what this movement is all about — acknowledging that we can be better, and coming to a place where we are better.”
Similarly, Dr. Gordon’s work within the school of medicine is focusing on accelerating a number of existing efforts to address structural racism in recruitment and retention, climate and culture, and research and educational programs, with accountability at the core of the school’s efforts. “Wherever goals are set or data is evaluated, we need to have true accountability. That is true for our leaders and for all individuals. It is everybody’s responsibility to fix the problem,” she says. “We are an outstanding institution, but we can be better. To really live up to our reputation and national rankings in clinical care, research and education, we have to have an environment in which every individual is welcomed and heard, in which we commit ourselves to education about past inequities and to addressing and responding to current challenges. This,” Dr. Gordon says, “is our imperative.”
CHANGE DOESN’T HAPPEN IN A VACUUM, and rarely does it come about by one person’s hand. At UCLA, there are many people involved, both within the health system and the school of medicine. For many of those involved in this effort, such a movement has been a long time coming. And while the COVID-19 pandemic has been a mirror held up to the face of health care inequity in this country, it was the killing of George Floyd at the hands — rather, under the knee — of a police officer in Minneapolis on May 25, 2020, that was the catalyst for this push forward.
“This is not the first time that we have seen a Black man killed. But this ripping off of the BandAid has given way to efforts such as those we are undertaking at UCLA,” says Clarence H. Braddock III, MD, MPH, vice dean for education at the David Geffen School of Medicine at UCLA and executive director of the Anti-Racism Roadmap, which is described as a “path to ensuring racial justice, equity, diversity and inclusion.”
“Without a truly inclusive culture change, we’re not really going to move the needle,” Dr. Braddock says. “As we think about the history of racism in America, about issues of whiteness in America, these are things we’re not used to talking about in an open and frank way. A large part of our challenge is answering the question: How do we get comfortable being uncomfortable with topics that we’ve never really talked about before? The work of dismantling structural racism is very personal work.”
While discussions around such potentially hot-button topics are not easy to have, they are essential for there to be movement forward. Since the killing of George Floyd, “We have spent months reading, conversing and reflecting with as much discomfort and humility as possible on how we have fallen short on being an anti-racist school and what we can do to ensure that we become actively anti-racist and anti-discriminatory,” says Kelsey C. Martin, MD, PhD, dean of the David Geffen School of Medicine at UCLA. A central focus of those discussions has been on how to increase the diversity of trainees, staff and faculty “to truly change the face of academic medicine and make all individuals who are dedicated to our mission of advancing science and medicine feel welcome and supported,” she says
Addressing these issues is not new for the school of medicine; it has had an Office of Equity, Diversity and Inclusion, under Dr. Gordon’s leadership, for more than 10 years. In November, the school and UCLA Hospital System furthered that ongoing effort by together launching a new Health Equity and Translational Social Sciences Research Theme to promote equitable care by studying and developing new models and training to provide whole-person care that integrates social interventions with medical care. The work of the new research theme will not be limited to the school of medicine and health system; it “will build collaborations among social scientists on the Arts and Sciences campus, life scientists, and clinicians and clinical researchers in the medical school, as well as develop partnership projects within the UCLA Health System and throughout the Greater Los Angeles community that integrate social interventions with medical care,” Dr. Martin says. “The theme will train the next generation of clinicians and researchers to advance health eq - uity by addressing social determinants of health and structural racism.”
The school also has launched a national search for a vice dean for justice, equity and diversity inclusion. As Drs. Martin and Braddock note, the discussions can be uncomfortable. “Nobody likes to talk about racism,” says Keith C. Norris, MD (FEL ’85), PhD, professor of medicine and vice chair for equity, diversity and inclusion in the UCLA Department of Medicine. “We talk about the structures of racism because the notion of having personal responsibility for racism shuts us down. It is true that nobody in the room during these discussions owned slaves or created the institutional structures of racism. But racism is all our problem to solve.”
And while most physicians feel that they are not racially biased, “data shows that there are significant unconscious biases in the medical community,” Dr. Norris says. “A Harvard study suggests that doctors carry more implicit bias than in other professions. These biases can have a major impact on the delivery of equitable care.”
Such biases also can have a significant impact not just on patients, but also on colleagues of color. “As a Black woman (and mother, wife and academic) in America, I ask you to put aside your discomfort and welcome these conversations,” Dr. Folasade May wrote to her peers in the online publication Healio. Silence, she says, is a problem. “I feel that many of my colleagues think they are avoiding undue strain on our relationship by not discussing the current racial climate for fear of being clumsy or even offensive. In reality, however, the omission of a stance against racism can be more harmful to the relationship in the long run. … Only by breaking the silence on issues of race and racism and shifting from words to actions can we move forward as a scientific community.”
A significant framework for that ongoing discussion must be around an internal realignment of priorities to address institutional inequities, Dr. Norris says. “My current focus is on changing policies and practice in medicine. There must be diversity among those at the hiring table. UCLA is a big place, yet not many minorities are asked to sit on the committees where hiring decisions are being made, in large part because there are so few minority faculty at UCLA.”
Increasing faculty diversity is an important goal, but so, too, is hiring and elevating faculty of color to leadership positions. “I have seen efforts being made in diverse staffing, but what about in leadership?” asks Dr. Wyatt, who has been a faculty member in the Department of Psychiatry and Biobehavioral Sciences for more than 40 years. “Young people coming in are confused about the expectations and the path to get ahead. As re - searchers, we know how to teach about structural racism, but as an institution, we have not dealt with those structures,” she says. “It will take real courage to make systemic change.”
PART OF THAT SYSTEMIC CHANGE MUST COME IN ATTRACTING A MORE DIVERSE POOL of minority students to health care. As Dr. May noted in Healio, “Blacks are 12.7% of the U.S. population, but only 5% of physicians and a paltry 0.7% to 2.9% of faculty in STEM (science, technology, engineering and math) fields. America has produced fewer than 100 Black females with PhDs in physics.”
The pipeline, Dr. Norris says, is not only broken, it is unrealistic. “Mostly at the undergraduate and medical school level, there are special programs to help level the playing field for future doctors, but there have not been enough changes in the K-12 education system,” he says. “Without a plan of action, the numbers of Black and Latino physicians and researchers will not grow. Too few make it to a ‘pipeline’ program, and the fact that such programs even exist says that, as a society, we have been, and continue to be, unwilling to fix inequities in K-12 education.”
Xavier E. Cagigas, PhD, a clinical neuropsychologist and associate director of the UCLA Hispanic Neuropsychiatric Center of Excellence, agrees. He has worked with other bilingual and bicultural faculty, staff, interns, postdoctoral fellows and doctoral students to create the nationally recognized UCLA Cultural Neuropsychology Program. “Most people don’t know that in Los Angeles County, Latinos make up nearly 50% of the population,” Dr. Cagigas says. “In L.A. County, non-Hispanic whites are actually in the minority, 26.1%, but none of the research, service-delivery or teaching models are structured to reflect the health needs of our diverse population. It is time to build a better science model and workforce that address the actual cultural and linguistic needs of our Latina/o communities, who, together with other historically underrepresented minorities, make up approximately 75% of L.A. County and an exponentially growing proportion of the United States.”
AT ITS CORE, ADVANCING HEALTH EQUITY AND INCLUSION is about improving health outcomes for all patients. To accomplish that, improving access to care is key. “Excellence in clinical care is a central tenet of our mission, and we want to make sure that we are providing equitable care to all patients,” Spisso says. “We are committed to serving our Greater Los Angeles community, which includes expanding our clini - cal services to Medi-Cal patients.”
According to the California Department of Health Care Services, as of July 2020, the most current data available, there were more than 3.8 million people in Los Angeles County — about 38% of the population — enrolled in Medi-Cal, the state’s health care safety net. Spisso said that to expand access to UCLA’s tertiary and quaterna - ry care services to more of those patients, UCLA Health signed a major contract with the largest Medi-Cal provider in the region.
Another avenue to expand access to care is through the wider adoption of such newly emerg - ing tools as telemedicine, an area that experienced explosive growth during the pandemic. Alejandra Casillas, MD, MSHS, assistant professor-in-resi - dence of medicine, is a health-services researcher focusing on digital health care access and inequi - ties. “We know it doesn’t take care of everything — there will always be a need for care in a brickand-mortar clinical setting — but digital tools like telemedicine can be effective in delivering care for underserved populations,” she says.
This can be a particularly beneficial option for patients who have transportation obstacles or who otherwise might have to take a day off of work to get to an appointment. “Digital delivery of care can level the playing field,” she says.
ALL THAT UCLA HEALTH SYSTEM AND THE DAVID GEFFEN SCHOOL OF MEDICINE AT UCLA ARE DOING to address historic racial disparities in health care is taking place against the backdrop of the COVID-19 pandemic. Now, with vaccines approved and a nationwide inoculation program accelerating, a key effort will be to get the medicine into the arms of people who need it most.
Dr. Mays, of the public health school and special advisor to UCLA Chancellor Gene D. Block on Black life, worked with Naveen Raja, DO, of the Office of Health Informatics and Analytics and the COVID-19 vaccine team at UCLA Health System, to support a vaccine-distribution system through its hospitals and more than 180 commu - nity clinics. The program utilizes an equity-based model of medical vulnerabilities and social-risk factors she developed with Paul M. Ong, PhD, di - rector of the Center for Neighborhood Knowledge in UCLA’s Luskin School of Public Policy, and colleagues in the policy school. “Equity in the distribution of the vaccine must move beyond merely people’s health status but also must take into account the extent to which their ability to adequately follow public health protections are thwarted by their built environment, not having access to health care or information, or even running water,” Dr. Mays says.
UCLA also has taken the lead on a National Institutes of Health (NIH)-funded project that brings together 11 academic institutions in Cali - fornia and their community partners to develop a community-engaged approach to address the impact of COVID-19 on vulnerable populations across the state.
The COVID-19 California Alliance, or STOP COVID-19 CA, is part of the NIH’s broader Com - munity Engagement Alliance Against COVID-19 Disparities. The partnership is a joint effort among five UC medical campuses, two non-medical UC campuses and four other leading academic institutions in California. “This important col - laboration will include 11 major institutions with highly innovative community-partnered research projects,” says Arleen F. Brown, MD (FEL ’98), PhD, professor of medicine and co-leader of the Community Engagement and Research Program at the UCLA Clinical and Translational Science Institute. “These institutions reside and work in diverse communities with high rates of COVID-19 infections and complications across the state. The community input makes all the difference in these projects,” she says.
Each site within the alliance will leverage its own unique community partnership networks and insights to address local problems. In Los Angeles, for example, investigators plan to run in-depth virtual focus groups with multiethnic communi - ties to identify barriers and challenges to inclusive vaccine development and vaccination. Another project will assess racial and ethnic attitudes among high-risk veterans that might prevent them from accepting a potential vaccine, with the aim of developing messaging to encourage vaccination among this group. The lessons learned from these efforts will help to identify opportunities to apply innovative approaches statewide and nationally.
“Black, Latino and Indigenous populations account for nearly half of all reported cases of COVID-19 in the United States,” says Dr. Norris, who is co-leader of the project. “The goals of STOP COVID-19 CA are to work with this network of partnerships across the state to reduce disparities in knowledge of COVID-19; increase participation of all Californians, including underrepresented populations, in prevention, vaccine and therapeutic trials; and improve the uptake of approved vaccines.”
CHANGE IS NEVER EASY, DR. BRIGGSMALONSON CONCLUDES, and it may arrive in fits and starts. But change, she says, must happen. “Over the past months, we have started to reflect on our blemishes, but, also through these reflections, we have started to identify new solu - tions and novel approaches, and raise awareness to challenge the status quo so that we can transform into an organization that is rooted in equity and bound by our common humanity.
“The work we are doing,” Dr. Briggs-Malonson says, “is imperative for us to dismantle the invisi - ble barriers that have prevented us from advancing racial equity for our students, trainees, faculty, staff and patients. Now this is our time to take action to build an equitable future for each other and for those who we serve.”