Scientists at the UCLA Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research have been awarded a $4.6 million grant from the California Institute for Regenerative Medicine – also known as CIRM – to support a phase I clinical trial of a novel treatment for advanced sarcomas and other cancers with a specific tumor marker called NY-ESO-1.
Directed by Dr. Theodore Scott Nowicki in collaboration with Dr. Antoni Ribas, the trial will test a therapeutic approach that genetically engineers each patient’s own blood-forming stem cells to produce cancer-fighting immune cells called T cells.
The T cells used in the treatment will be modified to target NY-ESO-1, a protein that is highly produced by tumor cells of many cancers including melanoma and sarcoma. Ten to 20 percent of all cancers and 80 percent of synovial sarcomas have the NY-ESO-1 tumor marker. The expression of this protein almost exclusively occurs in cancer cells, making it a perfect target to train the patient’s immune system to find the tumor cells and eliminate the cancer.
Sarcomas account for one percent of all adult cancers and 15 percent of all pediatric cancers diagnosed annually in the United States. They generally fit into one of two categories: soft tissue sarcomas, which begin in fat, muscle, nerves, blood vessels and other connective tissues; and osteosarcomas, which begin in bones and are often diagnosed in children, teenagers and young adults. Between 25 to 50 percent of sarcoma patients treated with conventional methods (surgery, radiation and chemotherapy) go on to develop metastatic disease, meaning the cancer spreads to other parts of the body. Patients with metastatic sarcoma have very few treatment options, none of which has been proven to increase survival.
“Sarcomas are difficult to treat because of their rarity and diversity—the cancer has more than 50 distinct subtypes,” said Nowicki, a fellow physician in the UCLA David Geffen School of Medicine division of pediatric hematology/oncology and a Pediatric Scientist Development Program Scholar. “Conventional treatments such as chemotherapies target tumors, and despite decades of research, a single therapy that works across all sarcoma subtypes has not been developed. Immunotherapies hold promise in treating this cancer because they can empower the immune system to fight many different subtypes of the disease.”
The clinical trial involves a dual approach intended to provide patients with both short and long-term immune response to cancer. Mature T cells, as well as blood-forming stem cells – which continually create all types of blood cells including T cells – will be collected from each participant’s blood. In the laboratory, the research team will insert a gene for a receptor to the cancer marker NY-ESO-1 into the participants’ own blood-forming stem cells. It is expected that the genetically modified stem cells will generate a continual supply of T cells that are programmed to recognize and kill the cancer by identifying cells with NY-ESO-1. It takes time for these T cells to mature, so to provide a population of immediately available cancer-fighting cells, the team will also genetically modify each patient’s own mature T cells to recognize the NY-ESO-1 tumor marker.
Trial participants will receive transplants of their genetically modified blood-forming stem cells and mature T cells on consecutive days. Ribas, a professor in the UCLA David Geffen School of Medicine departments of medicine, surgery, and molecular and medical pharmacology and a member of the UCLA Jonsson Comprehensive Cancer Center, has shown in previous clinical trials that this initial force of modified mature T cells provides an immediate treatment. While the modified mature T cells begin fighting the cancer upon transplantation, the modified blood-forming stem cells will have sufficient time to generate an on-going supply of new modified T cells, resulting in a lasting immune response to the cancer.
Engineering T cells with cancer-fighting receptors is already a promising area of cancer research. This method — known as adoptive T cell immunotherapy — typically involves collecting T cells from the circulating blood of patients with cancer, genetically engineering the T cells in the lab with a cancer-finding receptor and transfusing the modified cells back into the patient. This produces a short-term immune response that effectively reduces cancer cells. However, adoptive T cell immunotherapy has limitations: people with cancer might not have enough T cells for the approach to work and once transplanted back into patients, the number of modified T cells declines over time since they cannot self-renew and often the cancer recurs.
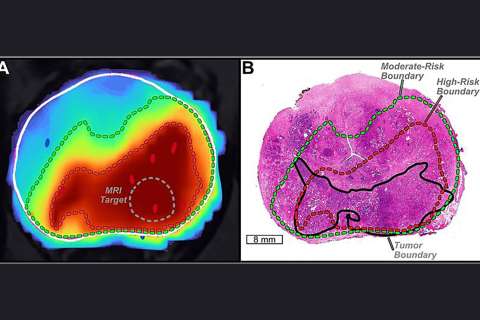
This trial will use positron emission tomography (PET) scanning, which is a noninvasive imaging technology that scans for diseases in the body and shows how organs and tissues are functioning. Each trial participant will undergo regular scans to track the engineered blood-forming stem cells and T cells to make sure the cells function as intended. If the cells behave abnormally, a drug can be administered to kill only the engineered cells. This part of the trial helps to ensure the safety of the patients.
This treatment platform is already being deployed in a related trial focused on multiple myeloma, which launched in September 2017 and is led by Ribas, who is also Director of the UCLA Parker Institute for Cancer Immunotherapy. That trial is funded by a $20 million grant from CIRM and support from the UCLA Broad Stem Cell Research Center. CIRM has been supporting Ribas’ work since 2008, beginning with a $3.07 million New Faculty Award that enabled him to develop the technology to deliver T cell receptor genes into blood-forming stem cells.
“This promising trial marks the culmination of CIRM and the stem cell center’s longtime support of Dr. Ribas’ work, which has been critical to moving this innovative platform from the lab to the clinic,” said Dr. Owen Witte, founding director of the UCLA Broad Stem Cell Research Center and professor of microbiology, immunology and molecular genetics.
The trial, also supported by the CIRM-funded UCLA-UCI Alpha Stem Cell Clinic, has received approval from the U.S. Food and Drug Administration to begin enrolling patients. Participants must meet several criteria to be eligible for the trial, including: testing positive for the NY-ESO-1 tumor marker and testing positive for a specific type of immune system called HLA-A2.1. Approximately 40 percent of the major western world ethnicities have the HLA-A2.1 immune system type.
To learn more about this clinical trial, visit its page at clinicaltrials.gov. If you think you might be eligible to enroll, please contact Project Scientist Paula Cabrera by email at [email protected] or by phone at 310-206-2090.
The grant was announced at a meeting of CIRM’s governing body, the Independent Citizens Oversight Committee, where two additional grants for projects involving UCLA faculty were also announced. Dr. Donald Kohn, a professor of pediatrics and microbiology, immunology and molecular genetics at the David Geffen School of Medicine at UCLA and member of the UCLA Broad Stem Cell Research Center, is a collaborator on both grants. The first grant will enable Rocket Pharma Inc. to launch a clinical trial of a gene therapy for Leukocyte Adhesion Deficiency, a rare genetic immune system deficiency. The second grant will fund a UC San Francisco-led team’s efforts to develop a patient-specific stem cell treatment for sickle cell disease using the CRISPR-Cas9 genome editing tool and obtain FDA approval to conduct a clinical trial.