UCLA and Caltech researchers have developed a technique that shows promise for preventing drug resistance in people with glioblastoma, the most common and deadliest type of brain cancer.
Drug resistance is one of the primary obstacles in treating glioblastoma — it is extremely common and affects virtually all people with the disease. But there is no consensus on why the body stops responding to treatment after a period of time, and scientists don’t yet have a tool for predicting drug resistance during the early stages of treatment.
The new technique uses penny-sized microfluidic chips that are equipped with minuscule DNA “bar codes,” which are no bigger than a single cell.
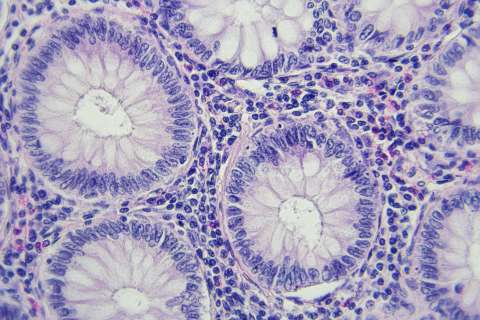
Glioblastoma tumors can grow rapidly and spread throughout the brain. The aggressive behavior is triggered by genetic mutations that cause the tumor cells’ protein signaling networks to become overly active. As a result, glioblastoma cells continuously receive signals that make them grow, divide and invade healthy tissue in the brain.
The current treatments for glioblastoma are designed to disrupt specific elements of the protein networks and to block the signaling that powers the tumor cells. But even when that approach is successful, it usually only works for a short time before the body becomes resistant to the treatment.
A paper about the new approach was published in the journal Cancer Cell. The research was led by James Heath, co-director of the UCLA Jonsson Comprehensive Cancer Center’s Nanotechnology Program. Heath and his team looked at how glioblastoma responded to a drug called CC214-2, which targets a signaling protein called mTOR. Mice with glioblastoma initially responded to CC214-2, but after a month they started to resist the drug, and their tumors began to grow again.
The researchers collected information from the microfluidic chips, which allowed them to anticipate resistance from a single or combination cancer treatment. They also found that within only two days after administering CC214-2, the cancer cells were adapting to the drug, and their ability to adapt foreshadowed full-scale drug resistance.
The cancer cells’ response to the drug was analogous to how automobile traffic responds to a road closure — they simply found new molecular routes through which to maintain their hyperactive signaling. In other words, the very cancer cells that had responded to the drug initially were the same ones that became resistant to the drug over time.
The single-cell analysis also showed the researchers the specific “traffic patterns” the cells used to get around the inhibiting influence of the drug, which gave the scientists key insights about the drug combinations they could use to inhibit the mTOR protein and the proteins that provided the alternate signaling routes.
Previous findings had suggested that drug resistance against targeted inhibitors for glioblastoma or other tumors likely occurred from one generation of cancer cells to the next — meaning that the cells could randomly develop genetic mutations that either disrupt the drug binding or counteract its effects — rather than because of individual cells’ ability to adapt. The new study was one of the first to show that cancer cells can adapt to drug treatments without genetic changes by rewiring their internal signaling circuitry.
“By sensing this adaptation so early, we were able to anticipate and treat drug resistance,” said Heath, who is also the Elizabeth W. Gilloon Professor of Chemistry at Caltech.
The scientists used their single cell measurements to predict three drug combinations that would stop tumor growth over the long term, as well as four drugs or drug combos that would likely have no effect. While testing all seven predictions, they found that each prediction was correct. The findings have also shown positive results in mammal models with melanoma.
The research team also included Dr. Tim Cloughesy, a member of the Jonsson Cancer Center and professor and director of the UCLA department of neurology; Wei Wei, a first author of the study and an assistant professor of molecular and medical pharmacology at the David Geffen School of Medicine at UCLA; and Dr. Paul Mischel, a former UCLA faculty member who is now a professor at UC San Diego’s Ludwig Institute for Cancer Research.
The research was supported by the Ben and Catherine Ivy Foundation, the National Cancer Institute and the Jean Perkins Foundation.
Heath is the founder and a board member of Isoplexis, a company that is seeking to commercialize the technologies used in the study.