Repairing rather than replacing a diseased mitral valve often has greater benefit for patients, says UCLA Health’s chief of cardiothoracic surgery and recently designated mitral-valve repair reference surgeon Richard Shemin, MD. “There are advantages to maintaining one’s own tissue as opposed to having artificial tissue and an implanted device,” Dr. Shemin says.
Patients who receive mitral-valve replacement must regularly take anticoagulant drugs to prevent blood clots. Such a regimen is not required for patients who undergo mitral-valve repair. “In general, patients who are able to maintain a repairable valve do better long-term,” Dr. Shemin says.
The American Heart Association (AHA) recently named the surgery program led by Dr. Shemin as a reference center for mitral-valve repair, and it designated Dr. Shemin as a reference surgeon. UCLA’s program is one of only three in the western United States, and it is the only one in Southern California, to receive such a recognition. The designation also reflects the expanded options offered by UCLA Health to patients with mitral-valve disease, including the use of minimally invasive robotic approaches and the program’s emphasis on mitral-valve repair.
The mitral valve is one of two valves on the left side of the heart that help to keep blood flowing in the right direction. As blood collects in the left atrium, it flows through the mitral valve to fill the left ventricle — the main pumping chamber that ejects blood through the aortic valve into the body’s circulatory network.
A variety of factors can lead to mitral-valve disease. The most common is a degenerative condition that prevents the valve’s flaps from closing tightly, causing the blood to leak backward, or regurgitate. This leads to symptoms that include shortness of breath and fatigue, requiring surgery.
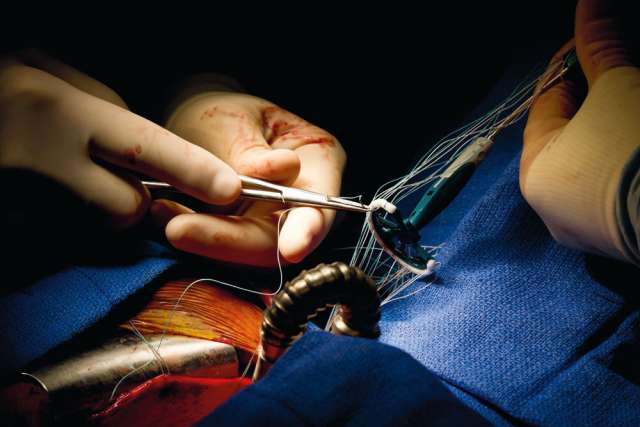
At a high-volume center such as UCLA, most diseased mitral valves can be repaired. Studies comparing mitral-valve repair with mechanical replacement involving an artificial valve have shown that repair procedures have a lower risk of complications and death. UCLA is also able to perform these complex procedures through minimally invasive, robotic surgical approaches that avoid the need for a sternal incision. “This leads to significantly less bleeding, less pain, more-rapid recovery and a better cosmetic result,” Dr. Shemin notes.
When mitral-valve replacement is necessary, UCLA is one of the first centers in the nation to implant Mitris Resilia, a mitral-valve device with an advanced tissue technology to improve the durability of the valve.
Beyond repair and replacement, UCLA’s portfolio of mitral-valve treatments includes nonsurgical interventions that patients may qualify for, such as MitraClip, a device introduced via a thin catheter that is threaded through the femoral vein in the groin to the left atrium, where it is deployed and attaches to the two leaflets of the mitral valve to clip them together and reduce the backflow of blood. The program also provides patients access to clinical trials of the latest technologies, including the HARPOON mitralvalve-repair system, which, rather than clipping the valve , uses transesophageal echocardiography guidance to place an artificial cord on the valve, pulling the leaflet of the valve back into position while the heart continues to beat.
“Patients diagnosed with mitralvalve disease have many more treatment options than in the past,” Dr. Shemin says. “They are best served being treated at a center of excellence, where everything from medical therapy through the variety of surgical therapies and advanced devices is offered, and there is a team of experts able to tailor the necessary care to each individual patient.”