Thrombectomy – pulling a clot out of a blocked brain artery – is now the gold-standard treatment for acute ischemic stroke and was invented at UCLA.
After the designation “thrombectomy-capable stroke center” (TSC) was rolled out in 2018 and volumes of the procedure steadily increased, UCLA researchers wanted to better understand the role of TSCs in the U.S. stroke care system.
“The idea for the study was based on the relatively newly introduced level of certification for stroke centers, which was launched due to the overwhelming evidence of the benefit of thrombectomy,” explains Radoslav Raychev, MD, assistant clinical professor of neurology at UCLA and lead author.
“At UCLA, we wondered, ‘What is the impact [of the designation]? How do we increase access to treatment?’ It inspired us to really look at the guidelines, the national database and the capabilities of thrombectomy-capable centers to understand whether this designation benefits stroke patients, and what the potential deficiencies are in other centers. Most importantly, we were looking to improve stroke care nationwide and worldwide.”
UCLA has pioneered systems of care processes in parallel with procedural and scientific innovation, notes Dr. Raychev, highlighting the institution’s ongoing interest in addressing stroke care beyond the doors of their state-of-the-art center.
Dr. Raychev, along with Jeffrey Saver, MD, director of the UCLA Comprehensive Stroke and Vascular Neurology Program, set out to explore the difference in quality of care and clinical outcomes of reperfusion therapies to restore blood flow among primary stroke centers (PSCs), comprehensive stroke centers (CSCs) and TSCs.
Center designations defined
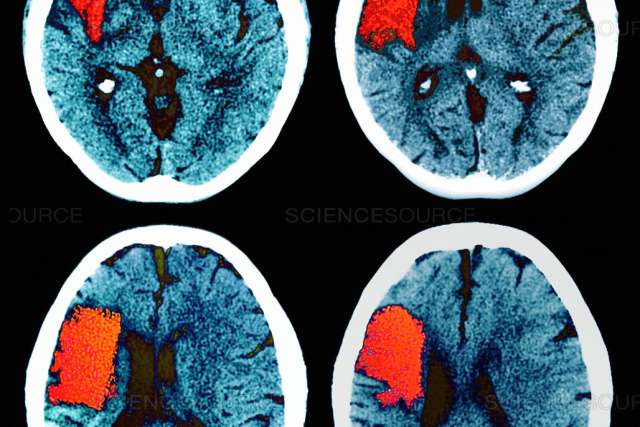
Each type of stroke center adheres to guidelines that are specific to their designation. At PSCs, the center provides primary stroke care. Ischemic stroke is treated with the well-established clot-dissolving medication known as tissue plasminogen activator (tPA), as opposed to more complex procedures.
The TSC designation supports the use of thrombectomy in those experiencing acute ischemic stroke, a minimally invasive surgery to remove a blood clot. CSCs administer tPA, perform thrombectomies and perform complex endovascular and open surgical interventions for hemorrhagic stroke patients.
“Prior smaller studies including all stroke patients have shown that CSCs and PSCs were fairly equivalent in terms of clinical outcomes. That is because CSCs were treating sicker patients,” Dr. Raychev explains. “No study looked specifically at reperfusion-treated stroke patients at these three designations and how they impacted patient outcomes.”
Study details and findings
Their observational cohort study of 84,903 reperfusion-treated patients recruited from the Get With The Guidelines–Stroke registry examined endovascular and/or intravenous reperfusion therapies at CSCs, TSCs or PSCs. Researchers were interested in timeliness of the interventions, successful reperfusion, discharge destination, discharge mortality and functional independence at discharge.
They found that TSCs and CSCs showed similar performance, and both exceeded PSCs in key reperfusion care quality and outcome metrics.
“First of all, we found that thrombectomy-capable centers performed at the same level of comprehensive centers. So the thrombectomy-capable designation is indeed beneficial,” says Dr. Raychev. “This is because the metrics that the TCSs have to adhere to are the same as the CSCs in terms of the procedure that needs to be performed.”
“While thrombectomy stroke centers were created to provide brain-saving clot retrieval procedures to stroke patients in regions without major comprehensive centers, there was concern that the outcomes in TSCs would be suboptimal,” says Dr. Saver. “Our study provides important reassurance that TSCs are capable of performing these procedures and managing patients post-procedurally.
“This finding will help increase access nationwide to this leading acute stroke therapy.”
The researchers also found that in the U.S., thrombectomy is often performed at PSCs — in some cases up to 100 per year, Dr. Raychev reports, noting the study’s median thrombectomy volume of 32 for PSCs. The requirement to be certified as thrombectomy capable is only 15.
“Virtually, almost all PSCs in this study were eligible to be thrombectomy capable, yet they’re not. That is a key finding of our study,” Dr. Raychev says.
“Considering that over one-fifth of all [endovascular thrombectomy] procedures during the study period were conducted at PSCs, it may be desirable to explore national initiatives aimed at facilitating the elevation of eligible PSCs to a higher certification status,” the authors note in their study, highlighting the value of advanced stroke center certification.
The conversion of eligible PSCs to TSCs to attain higher certification levels could potentially result in improved treatment and better clinical outcomes, Dr. Raychev concludes, because of the higher standards required for thrombectomy-capable certification.
“There should be uniform criteria, uniform adherence to these metrics and uniform efforts to designate centers that are meeting criteria to become thrombectomy-capable and improve their quality of care,” he says. “This study will have an important impact on regional and national systems of stroke care.”