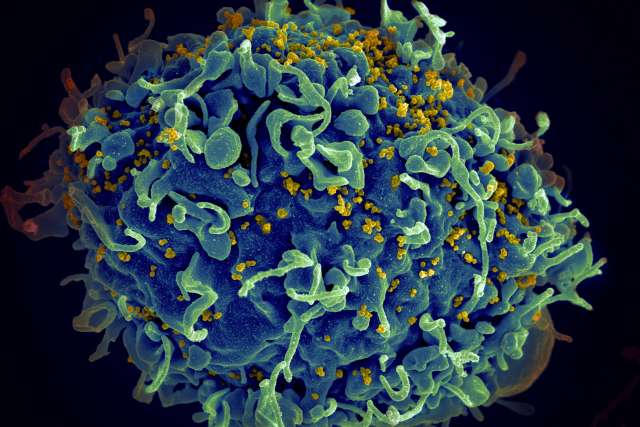
UCLA researchers presented today the first case of a U.S. woman living with HIV-1 that is in remission after she received a new combination of specialized stem cell transplants for treatment of acute myeloid leukemia (AML). The oral abstract was presented at CROI 2022, the Conference on Retroviruses and Opportunistic Infections.
This woman has been in remission of AML for 4½ years and has had no HIV rebound in the 14 months since antiretroviral therapy was stopped, said Dr. Yvonne Bryson, a distinguished professor and specialist in pediatric infectious diseases and HIV pathogenesis at the David Geffen School of Medicine at UCLA and the UCLA Mattel Children’s Hospital, who led the National Institutes of Health-supported, multicenter, observational study (IMPAACT P1107).
If HIV remission continues and she is determined to be cured, she would be only the third person to achieve cure and the first HIV remission to have been successfully engrafted with umbilical cord blood cells with a mutation that is protective against HIV-1 (CCR5-delta32/32 homozygous) combined with stem cells from an adult, haploidentical (“half-matched”) related donor. The two previous patients with HIV cure received adult donor cells – one from bone marrow and one from blood stem cells – that had the protective mutation, but no umbilical cord blood cells.
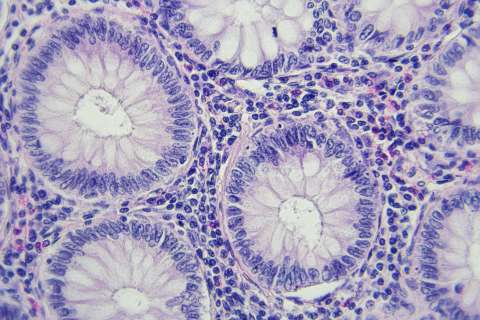
The woman is of mixed race who was diagnosed with acute HIV in 2013 and high-risk AML in 2017. She was successfully transplanted with cord blood cells having the HIV-protective CCR5-delta32/32 mutation and with adult stem cells from a related donor. She had rapid engraftment with 100% cord cells by day 100 post-transplant and did not experience graft-versus-host disease, as the two earlier patients did, and she remains clinically well, with no detectable evidence of HIV infection, the researchers said.
Although stem cell transplantation is not a therapy for HIV, its effects in patients living with HIV and undergoing therapy for blood or lymph cancers provide researchers with insights and potential targets in HIV treatment.
“This study provides hope for the use of cord blood cells or a combination of cord blood cells and haploidentical (half-matched) grafts to achieve HIV-1 remission for individuals requiring transplantation for other diseases. It also provides proof that HIV-1 viral ‘reservoirs’ can be cleared sufficiently to afford remission and possibly cure in the setting of resistant target cells,” said Bryson, the protocol chair for the International Maternal Pediatric Adolescent AIDS Clinical Trials Network (IMPAACT), the organization conducting the observational IMPAACT P1107 study.
The CCR5-delta32 mutation is rare, but cord blood banks may provide a previously untapped resource, according to the researchers, and the combination therapy would enable clinicians to take advantage of the unique benefits offered by each type of graft for more diverse populations.
“Adult donor grafts provide many cells initially and rapid engraftment, but histocompatibility can be an issue leading to risk of graft-versus-host disease. Umbilical cord blood grafts have a lower cell dose and take longer to engraft, but they can be banked for ready availability, and they pose less risk for GVHD,” Bryson said. “With the combination, the adult graft provides accelerated engraftment until the cord graft takes over.”
Bryson leads the IMPAACT P1107 study with protocol virologist and scientific committee chair Deborah Persaud, a pediatric infectious disease specialist at Johns Hopkins Medicine. The protocol team includes Anne Coletti, Koen Van Besien, Savita Pahwa, Renee Browning, , Lawrence Petz, Marshall Glesby, Theodore Moore ,Fredrick Bone, Amanda Golner, Rohan Hazra, Nicole Tobin, Meredith Warshaw, Patricia Anthony, Dwight Yin and Elizabeth Smith.
Clinical research site investigators at Weill Cornell Medical College include JingMei Hsu, Koen Van Besien from the transplant team, and Marshall Glesby,infectious disease , and collaborators include Lawrence Petz, StemCyte; Marcie Riches, Center for International Blood and Marrow Transplant Research (CIBMTR); and John Mellors, AIDS Clinical Trials Group (ACTG).
Additional contributors include Ruth Cortado, Bryson Laboratory at UCLA; Dianna Hoeth, Mellors Laboratory at the University of Pittsburgh; Suresh Pallikkuth and Margaret Roach, Pahwa Laboratory at the University of Miami; and Ya Hui Chen, Adit Dhummakupt, and Joseph Szewczy, Persaud Laboratory at Johns Hopkins University.
IMPAACT P1107 is funded by the U.S. National Institutes of Health. Overall support for the International Maternal Pediatric Adolescent AIDS Clinical Trials Network (IMPAACT) is provided by the National Institute of Allergy and Infectious Diseases (NIAID) with co-funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the National Institute of Mental Health (NIMH), all components of the National Institutes of Health (NIH), under Award Numbers UM1AI068632-15 (IMPAACT LOC), UM1AI068616-15 (IMPAACT SDMC) and UM1AI106716-09 (IMPAACT LC), and by NICHD contract number HHSN275201800001I. NIAID funding for the ACTG Weill Cornell Medicine – Rutgers New Jersey Medical School Clinical Trials Unit was provided under 5UM1AI069419.
The authors report no additional disclosures or potential conflicts of interest.