Before the COVID-19 pandemic, waking up with the sniffles or a cough meant you probably caught a cold, or at worst, the flu.
Nowadays, those symptoms could mean you’ve joined the more than 50 million Americans who’ve contracted COVID-19.
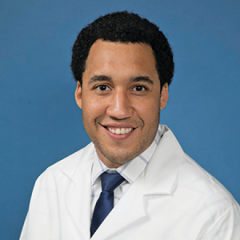
Omai Garner, PhD, director of clinical microbiology for UCLA Health, had these same concerns when he woke up one recent morning with a stuffy nose.
Dr. Garner has been at the forefront of COVID-19 testing research since the pandemic started. When his respiratory symptoms surfaced, he immediately wondered: “Is it a cold or COVID?”
“Some of my friends and colleagues have had breakthrough cases, and it started out with this runny nose, scratchy throat thing,” Dr. Garner says.
“Could it be allergies? Sure, it could definitely be seasonal allergies. Could it be a cold? Absolutely. There are plenty of colds circulating. Could it be COVID? What’s especially interesting about COVID, especially in young children or vaccinated patients, COVID comes on a lot like that.”
Dr. Garner keeps COVID-19 antigen tests in his medicine cabinet at home for just such a circumstance. When symptoms are present, antigen tests can provide some insight into whether COVID-19 is the cause, he says.
Antigen vs. PCR tests
While polymerase chain reaction, or PCR, tests are the gold standard in COVID-19 testing, they must be performed by a laboratory. Antigen tests, on the other hand, are over-the-counter at-home tests that quickly screen for proteins in SARS-CoV-2, the virus that causes COVID-19.
“Antigen tests have a reasonable accuracy,” Dr. Garner says. “By reasonable accuracy, I’m putting this around 80% accurate when a person is symptomatic in their first three to five days of illness.”
Those first symptomatic days are when viral load, or the amount of virus present in the body, is highest.
“The true difference between the antigen test and the PCR test is really just how much virus it can measure,” Dr. Garner says. “It takes a lot of virus to make an antigen test positive.”
PCR tests are much more sensitive, which allow them to detect asymptomatic infection. But for cold symptoms that could be COVID-19, a home antigen test is a good first step, Dr. Garner says.
“If you take the antigen test and if it’s positive, my suggestion is to isolate and immediately follow up with a PCR test,” he says. “Because there are false positives on the antigen side.”
A negative result
Coughing and congested, Dr. Garner tested himself at home and was relieved to get a negative result. If his symptoms had worsened the next day, however, he would have sought the more sensitive, professional test.
“If a person has early cold symptoms and the next day wakes up with a fever, even if the antigen test was negative they should go get a PCR,” he says.
Not everyone can afford to keep antigen tests around the house, Dr. Garner notes, since a two-pack of the single-use tests costs at least $25 at most drugstores. But for those who can, it’s a good idea to get insight about symptoms, particularly as cold and flu season arrive.
Especially if you’re the parent of a toddler, he adds.
“Mainly because my 2-year-old started going to the park and started playing with his 2-year-old friends, I’m on my fourth cold now,” Dr. Garner says. “It just became apparent to me how useful having that test in the medicine cabinet was going to be.”
Keep up to date on the latest COVID-19 vaccine information.
Related articles
How viruses, including the coronavirus, make you sick
Will children 5 to 11 soon be able to get their COVID-19 vaccines?
COVID-19: Track the latest developments and look back at how the pandemic evolved



