Losing the sense of smell is one of the symptoms associated with COVID-19, but many people live with a minimized or lost sense of smell from other causes too.
According to the National Institutes of Health (NIH), studies conducted before the COVID-19 pandemic found that one in eight adults (12%) older than 40 has measurable smell dysfunction. About 3% of Americans have anosmia (no sense of smell) or severe hyposmia (minimal sense of smell).
Living with a reduced or lost sense of smell can greatly affect your health, happiness and general quality of life, and it can happen to anyone. We’ve answered the most common questions about smell and your health, in case you or a loved one experience a loss of smell.
Why is smell important?
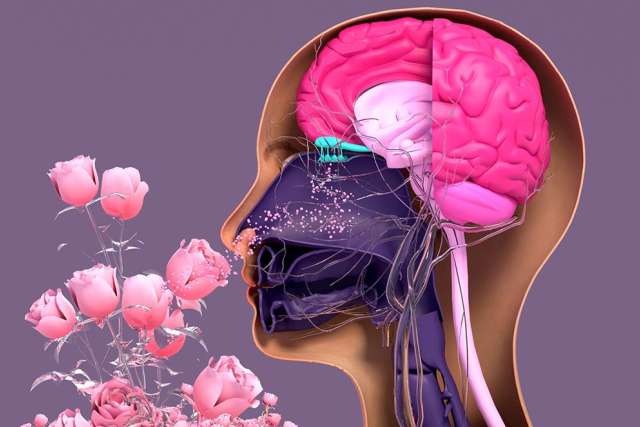
Your olfactory system, the part of the body that serves the sense of smell, has many important functions. It helps people determine what to eat, influences taste and affects socialization. Smell also provides a warning for hazardous events such as fires or gas leaks.
What causes smell loss?
For some people, their sense of smell may change or disappear but then return to normal. For others, the loss may be permanent.
Temporary loss of smell may result from:
- Cancer treatments, including radiation and chemotherapy
- Harmless growth in the nose or sinuses, called a polyp
- Medications, such as antibiotics or blood pressure medication
- Sinus or upper respiratory infections, such as a cold, the flu or COVID-19
- Smoking, which makes you six times more likely to have a poor sense of smell
The causes of permanent loss of smell may include:
- Age, especially after age 70
- Conditions affecting the nervous system, such as multiple sclerosis, Alzheimer’s disease and Parkinson’s disease
- Exposure to certain chemicals, when exposure occurs for a long period of time
- Head injury, which can damage the nerves related to smell
How does loss of smell affect your health?
A loss of smell can affect how you live and how you feel. No matter what level of impairment you experience, you’ll see the effects in many areas of your health, including:
Mental health
Your sense of smell is closely connected to the part of the brain involved in behavioral and emotional responses. That’s why certain odors spark strong emotions, influence behavior and trigger memories. Smell can also determine your attraction to other people.
People with anosmia may feel disconnected, indifferent, anxious or depressed. Studies show that a loss of smell can negatively affect relationships and increase feelings of isolation. In people with olfactory dysfunction, symptoms of depression often worsen with the severity of smell loss.
Nutritional health
When your sense of smell alters your perception of food, it can greatly impact your food choices. Smell helps us determine whether a food is ripe or has gone bad. Without that aid, you are more likely to ingest food that may make you sick.
A loss of smell also throws off your sense of taste. According to the NIH, without smell, humans detect only five basic tastes: sweet, salty, bitter, sour and savory (umami). Your brain uses both taste and smell to create the perception of a variety of different flavors. Without the element of smell, your food may taste “off,” causing you to lose interest in eating, reduce your appetite or affect your eating habits.
Physical safety
A loss of smell can leave you vulnerable to dangerous events such as fires and gas leaks. Typically, an odor of smoke or toxic fumes is the first warning of danger. Without that warning, the chance of safe escape and minimal exposure decreases. A 2014 study found people with anosmia to be twice as likely to suffer from hazardous situations as people without smell loss.
What if you have a change in smell or taste?
If you notice a diminished smell or a change in how your food tastes, make an appointment with your primary care provider, who can perform a “scratch and sniff” smell identification test to evaluate your symptoms.
Your primary care physician may refer you to an otolaryngologist, who specializes in diseases of the ear, nose, throat, head and neck (often called an “ENT”). A proper diagnosis is vital to managing or treating the underlying cause of your loss of smell.
Is there treatment for loss of smell?
If you’ve lost your sense of smell temporarily, things may smell different when the sense returns. Certain odors may register as unpleasant or altered from how you previously perceived them. The good news is that there are treatment options to help you regain your full sense of smell, including:
- Smell training, which helps people relearn certain odors by sniffing them regularly in a controlled environment
- Steroids, if your smell loss is due to inflamed nose cells, which is common for people in early stages of a COVID-19 infection
Researchers are also working to find new ways of activating the sense of smell for people with anosmia. Treatments including electrical stimulation and olfactory implants may one day be used to trigger the brain’s response to smell.
If you notice a loss of smell or a change in taste, make an appointment to see your primary care provider.