Functional Image-Guided Radiation Therapy
PET/CT
The UCLA Department of Radiation Oncology utilizes a state-of-the-art Positron Emission Tomography CT scanner (PET/CT) for the planning of your radiation therapy when it is appropriate. We are one of the few radiation oncology departments in the country that has a dedicated PET/CT scanner used solely for the purpose of planning radiation treatments.
What is a PET/CT?
A PET scan is a type of non-invasive nuclear medicine test that uses a modified sugar radioactive tracer (FDG) injected into your body. With special imaging equipment, it is possible to detect radiation from the administered radioactive agent and obtain images of the body. A combined PET/CT scanner allows us to obtain conventional anatomical information regarding your tumor and your normal organs, which allows us to customize the radiation fields specifically to you. In addition, the PET portion of your radiation simulation allows us to perform further refinements of your treatment by obtaining metabolic information regarding your tumor.
Why is a PET/CT better?
A combined PET/CT allows us to detect areas of your disease that would have otherwise been missed in a regular CT-based simulation, and in some cases differentiate the tumor from your normal tissue. The combination of a PET and CT scan provides both anatomical and metabolic information regarding your tumor and your body. Using this highly advanced technology, we ensure that we maximally target your tumor with radiation, and spare your normal critical tissues. In this manner, we expect that you will receive better efficacy in terms of tumor control as well as less side-effects with this form of radiation planning.
When is a PET/CT used?
A PET/CT simulation is often but not always used for cancers of the head and neck, cancers of the lung, cancers of the gastrointestinal tract, cancers involving the lymphatic system, as well as other cancers (Figure 1). There is compelling recent scientific evidence that using a PET/CT scan to plan radiation leads to improved tumor control and outcomes for patients. In collaboration with the Division of Nuclear Medicine at UCLA, we are leaders in the advancement of functional imaging such as PET imaging in improving outcomes in radiation treatments for cancer. Current projects include better ways of integrating PET in radiation treatment planning, as well as the use of new tracers in detecting cancer at an earlier stage. We believe that this will make them more amenable to treatment.
Our Experts
Radiation Oncologists
Michael Steinberg, MD
Percy Lee, MD
Physicists
Nzhde Agazaryan, PhD
Nuclear Medicine
Johannes Czernin, Ph.D
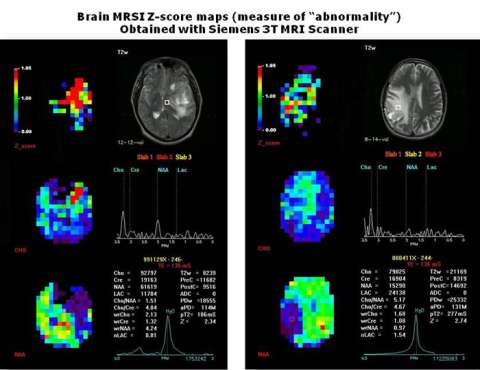
Figure 1: The images below represent different imaging modalities used by radiation oncologists to create a more personalized and informed treatment plan.
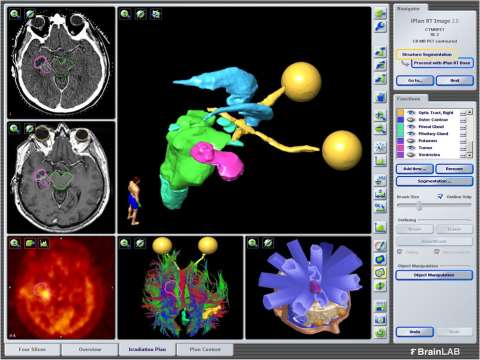
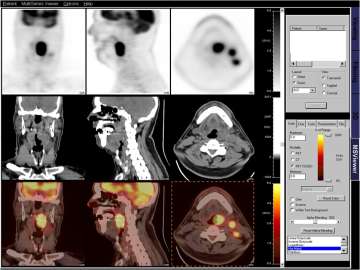
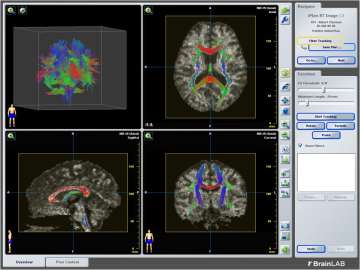
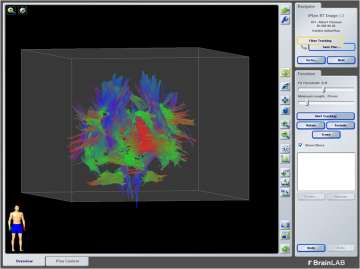
Figure 2: Magnetic Resonance Spectroscopic Imaging (MRSI). This type of imaging can can help indicate areas that are diseased which may not be visible with typical MRI scans. The color bar below shows levels of abnormality. Areas in red depict higher levels of abnormality.