Mission Pillars
Find your care
If you’re admitted to the hospital, your primary care physician will ensure that you receive care from a UCLA Health hospitalist. Please call us at 855-488-9550 if you have questions.
Clinical Care
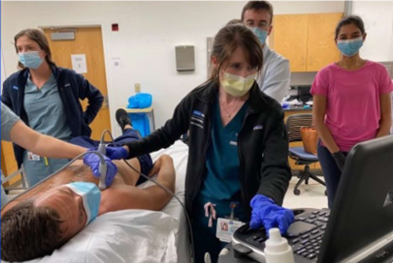
Procedures
Our UCLA Health hospitalists have strong in-hospital procedural support from our interventional radiology colleagues and a robust proceduralist service staffed by our hospitalists. The Procedure Service was started in 2015 as a part of the Hospitalist department in conjunction with the internal medicine residency program. It is staffed by a select group of hospitalists, dubbed "proceduralists," who have demonstrated an aptitude for procedures and teaching. The team is available for bedside, ultrasound-guided procedures including paracenteses, lumbar punctures, central venous catheters, and ultrasound-guided peripheral IVs. Hospitalists who are interested in joining the team receive extensive mentorship from senior proceduralists and complete procedure simulations in the simulation center. Once they demonstrate competency in performing procedures, they may become core members of the team with procedure service weeks integrated into their hospitalist schedule. Our proceduralists are also core educators who work closely with residents on the service and teach them best practices to help them build confidence in their bedside procedural skills. They also often help teach procedural skills in the medical school curriculum.
Medical Education
Medical Education
The UCLA Health hospital Medicine has a strong commitment to educating future generations of physicians. Our faculty play key roles in nearly every aspect of medical education in the UCLA David Geffen School of Medicine and the UCLA Internal Medicine Residency, as well as many initiatives outside the boundaries of these institutions. Hospitalists participate in preclinical medical school activities, such as small group learning, simulation, and lectures at the David Geffen School of Medicine. Some of our hospitalists work regularly with pre-clinical medical students as Educators for Excellence, where they meet weekly with a group of students to teach the basics of clinical medicine. Others are part of the Longitudinal Clinical Experience course, wherein a 3rd year medical student in their “Discovery” year is paired with faculty members to meet regularly in the clinical space. Others run individual simulations or other educational sessions. Our hospitalists also work closely with 4th year medical students on a variety of clinical rotations that range from classic sub-internships to an innovative Advanced Hospitalist elective where a 4th year medical student works 1:1 with direct care hospitalist.
Our hospitalist faculty are also very engaged in medical education within the UCLA Internal Medicine Residency Program and other residency programs in the Los Angeles area. UCLA Health hospitalists rotate on teaching services at multiple UCLA Health institutions, in addition to other community institutions, and are an integral part of the clinical educational experience of trainees. Beyond teaching on clinical services, our faculty are involved in a broad spectrum of residency medical education. They often lead noon conference, morning reports, UCLA Department of Medicine Grand Rounds, and other didactic curriculums. They have started innovative ultrasound and procedural electives. They are leaders of inclusive excellence, informatics, global health, evidence-based medicine and many other curricula. Our hospitalists have received many teaching awards for their work in these areas, and the department prides itself in supporting its faculty in their educational roles to allow for growth and innovation.
Point of Care Ultrasound (POCUS)
The UCLA Health Hospital Medicine is committed to advancing the use of Point of Care Ultrasound (POCUS) in clinical practice and teaching POCUS to the next generation of physicians. Our hospitalists faculty have the opportunities to build their POCUS skills through a variety of educational sessions organized by Drs. Daniel Kahn and Reece Doughty, the Director and Associate Director of Bedside Ultrasound Education. These range from online modules to hands-on didactics, to longitudinal image review and feedback. For those interested in teaching POCUS, there are multiple opportunities to teach internal medicine residents and medical students throughout the year.
Furthermore, we have the capability to upload POCUS images and videos to our electronic medical system to enhance patient care. We also maintain a UCLA POCUS website with extensive UCLA-specific and external ultrasound resources, a monthly ultrasound case series and journal club. Each year we work to continuously expand POCUS training and opportunities so that UCLA Health can continue to be a leader among academic institutions.

Simulation
It has been well-established that simulation is an effective educational tool to undergraduate and graduate medical training. As such, our hospitalist section is highly engaged in teaching through simulation in a variety of different settings. First, the David Geffen School of Medicine and the UCLA Internal Medicine Residency Program each have a robust curriculum of simulation training held in the recently renovated state-of-the-art Rosenfeld Hall simulation center. Students and trainees participate regularly in half-day sessions using high-fidelity mannequin simulators. These are regularly led by hospitalist faculty, and there is ample opportunity to do so throughout the year.
Additionally, our faculty are involved in curriculum design as well as the design of individual simulation cases. In addition to sessions held in the Rosenfeld Hall simulation center, a group of our UCLA Health hospitalists lead an innovative new simulation program called "in-situ simulations," through which residents at the UCLA Ronald Reagan Medical Center participate in short simulation cases in the hospital while on service. Virtually Reality simulation and other innovative simulation techniques are also being actively investigated by out faculty.



Research, Innovation & Scholarship
Several UCLA Health hospitalists are involved in research and scholarship, including in-clinical practices, medical education, quality improvement, bioinformatics, social medicine, value-based care and health services research. In alignment with the UCLA Department if Medicine strategic plan, we seek to increase the impact and profile of hospital medicine research both locally and nationally.
UCLA Health offers many services to researchers through UCLA Clinical and Translational Science Institute, including consulting in study design, datasets, and statistical analysis.
Publications by UCLA Hospital Medicine
Research Spotlight
Dr. Russ Kerbel's work on artificial intelligence models in early detection of sepsis was featured in the February 2025 departmental newsletter.
Dr. Rich Leuchter's work on the Next Day Clinic was a Top Research Presentation at the SMH Converge 2025.


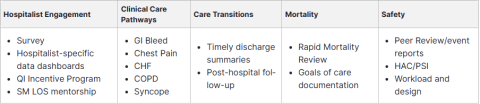
Quality Improvement
The goal of the UCLA Health Hospital Medicine Quality Improvement (QI) Program is to engage hospitalists in quality improvement through data-sharing, collaboration, training and mentorship aid to improve the quality and delivery of care in our hospitals. In keeping with the spirit of the UCLA Department of Medicine's core values, our work is focused in improving patient outcomes, educating future quality improvement leaders, and developing innovative solutions to system issues.
The section of hospital medicine has active initiatives in all areas of UCLA Health's MOVERS quality strategy: Morality, Outcomes, Value, Experience, Readmissions, and Safey. UCLA Health hospitalists also lead and participate in QI projects and committees through the department, hospital, faculty practice group. Formal Lean training is offered to all interested hospitalists in collaboration with UCLA Performance Excellence.
Inclusive Excellence & Community Engagement
Commitment to Inclusive Excellence and Community Engagement
UCLA Health hospital is committed to the principles of community engagement and inclusive excellence. For the past several years, we have made great strides to foster tangible improvements in these domains. We have re-structured our hiring and recruitment committee to provide more equitable and holistic evaluations while looking to improve the representation of equally qualified faculty from diverse backgrounds and life experiences. We actively teach about implicit bias to residents and students on our wards, in addition to our hospitalists. We are rolling out a longitudinal professional development curriculum to improve our hospitalists' knowledge and comfort with these topics as they relate to healthcare and medical education.
The section of hospitalist medicine is actively involved in and increasing our engagement with the community. any of our hospitalist work with the UCLA Homeless Healthcare Collaborative, a mobile outreach unit focused on caring for people experiencing homelessness where they are meeting patients in the streets, in encampments, or in shelters to deliver medical care and social services to those most in need. They can provide post-discharge follow up care for the unhoused population, facilitate improved medication adherence, and coordinate primary and specialty care.
Additionally, we have several individual hospitalists engaged in mentorship activities at the high school, undergraduate and medical school levels. The UCLA Summer Health Professions Education Program and the UCLA Premedical Enrichment Programs are both pipeline programs intended to improve access and matriculation of underrepresented minorities into top-tier medical schools, and hospitalists can provide invaluable mentorship for these students.
Dr. Veronica Ramiez, the clinical lead of our Downtown cohort, is actively supporting multiple learners and faculty of Hispanic descent though her involvement in groups such as "First-Gen", a UCLA undergraduate student group or first-generation Hispanics, and the Latino Medical Student Association (LMSA), with the goal of increasing representation of these historically underrepresented groups in medicine.
Other opportunities for community involvement include participation in health fairs such as Care Harbor, providing free medical, dental, and vision care to the uninsured, underinsured, and underserved in our communities. Some UCLA Hospitalist cohorts provide clinical care at MLKCH and Olive View-UCLA Medical Center, both of which are local safety net hospitals.
We understand that the health of our patients and the caliber of our medical education depend on optimizing community engagement and inclusive excellence in our clinical and teaching spaces and are this committed to continuing to develop and foster this culture within UCLA Health Hospital Medicine.
Global Health
Several of our hospitalist are active in global health education in our medicine residency program and at the David Geffen School of Medicine at UCLA. In the Internal Medicine Global Health Pathway, they mentor, train, and supervise medical students and residents during their clinical engagements at partner sites in Malawi, Peru, Thailand, and Shiprock, New Mexico. They contribute to a longitudinal global health curriculum for medicine residents, instructing on clinical as well as non-clinical topics such as ethics, decolonization and global health equity. They utilize their hospital medicine skills in their practice and instruction abroad and apply their expertise in areas such as POCS to patients in low-resource settings.

