Research
Find Your Care
Our interventional neuroradiology team has paved the way for interventional procedures, creating several of the devices and techniques widely used today. Call 310-267-8761 to learn more about our services.
RESEARCH PROGRAMS IN OUR DIVISION
Our Mission & History
Translational research is one of the primary functions of the Division of Interventional Neuroradiology. We identify limitations of the current technology through our daily clinical practice, and conduct a translational research to overcome the limitations.
The significant achievement of our translational research program is the invention of Guglielmi Detachable Coil (GDC) in 1990. GDC was designed, developed, and tested at the UCLA Rigler Radiology Research Center (currently called Translational Research Imaging Center /TRIC). The invention of GDC and subsequent development of aneurysm coiling technique pioneered by UCLA Interventional Neuroradiology induced a significant paradigm shift in the treatment of intracranial aneurysms throughout the World. (Guglielmi G, Viñuela F, Dion J, Duckwiler G. J Neurosurg. 75(1):8-14, 1991)
Not just a detachable coil, but liquid embolic material serves as an important tool in the field of neuro-intervention. Previous division chief, Professor Fernando Vinuela (currently Professor Emeritus of UCLA Interventional Neuroradiology) is one of the pioneers who introduced and popularized nBCA liquid embolic material for the embolization of brain arteriovenous malformations (AVMs). While nBCA remains as a great tool, one of the major limitations is its adhesive nature that prohibits long curative injection into brain AVMs. Therefore, it was very natural for us to participate in the development of Onyx embolic material, the world first non-adhesive liquid agent used for brain AVMs. Onyx embolic material was extensively tested at the UCLA Rigler Radiology Research Center. (Jahan R, et al. Neurosurgery. 48(5):984-997, 2001.)
Invention of MERCI Retriever, the first device approved in the United States to remove blood clots in patients suffering from acute stroke was also developed and tested at the UCLA Rigler Radiology Research Center by the lead inventor and our previous clinical faculty, Professor Y. Pierre Gobin. In the FDA approval clinical study, UCLA Radiology with a collaborative effort with UCLA Emergency Neurology and Stroke Neurology played a significant role. (Gobin YP, et al. Stroke 35(12):2848-54, 2004)
Invention of Matrix coil, the World first bio-active aneurysm coil was also developed at the UCLA Rigler Radiology Research Center with a new concept: instead of simply inducing clots in the aneurysm by the coils, Matrix coated with a bioactive polymer enhances a biologic healing of the aneurysm. Our previous faculty, Professor Murayama and previous chief, Professor Vinuela were the inventors and also principal investigators of this project. (Murayama Y, et al. Stroke. 34(8):2031-7, 2003)
Current Research Members of Interventional Neuroradiology
Gary R. Duckwiler, MD (Division Chief)
Reza Jahan, MD (Director, TRIC Lab)
Satoshi Tateshima, MD (Investigator)
Viktor Szeder, MD (Investigator)
May Nour, MD (Investigator)
Fernando Vinuela, MD (Investigator)
Inter-departmental Research Associations
Stroke Neurology
Vascular Surgery
Neuro-ophthalmology
Neuro-intensive Care
Neurosurgery
Head & Neck Surgery
Plastic Surgery
Pediatrics
Neuro-phathology
Current Projects
- New Device Testing
We are actively involved in the development of new neuro-endovascular devices with our industry partners (Medtronic, Stryker, Microvention, Blockade Medical, PulsarVascular, Reverse Medical, Medina Medical, Sequent Medical). Combination of our clinical quality flat panel DSA (Siemens Artis Zeego) and actively practicing neuro-interventionalsts performing those tests enables very realistic high quality evaluation of new devices.
We were involved in the development of many new devices such as Barrel Stent (Reverse Medical/Medtronic), MVP/Uno vascular plug device (Reverse Medical/Medtronic), PulseRider (PulsarVascular), Luna/Artisse (Nfocus/Medtronic), Web (Sequent Medical/Microvention-Terumo), Athena embolization coil (Medina Medical/Medtronic), Barricade Coil System (Blockade Medical), and Solitaire FR (Medtronic).



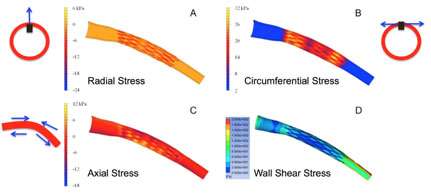
- Biomechanical Responses After Stent Deployment in a Curved Artery.
Placement of stent itself sometimes induces a stenosis in the artery. Interventional Neuroradiology and Neuro-pathology studied the biomechanical response of a curved artery to a Wingspan stent placement. We found that it is not just a radial force of the stent but stress concentration (all of radial, circumferential, and axial stresses) induced a strong biological response in the artery.
- Designing a Better Stent to Reduce Unfavorable Biomechanical Response
In order to reduce the unfavorable stress to the artery by a stent, we study various stent strut designs and the stress to the artery.

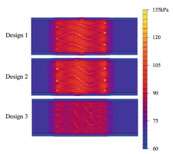
Von Mises stress distribution for the arterial tissue for the three different Designs 1–3
- Flow Diversion Stenting & Hemodynamics
We study hemodynamic effects of various stent designs particularly flow diversion stents such as Pipeline. The research helps for us to better understand the mechanism of aneurysm healing process after the flow diversion stenting, which will eventually improve the clinical outcome.


- Ischemic Complications of Soft Tissue Dermal Fillers
Soft tissue dermal fillers are used frequently in facial rejuvenation. As the use of fillers increases, accidental arterial injections and resultant ischemic complications including skin necrosis are becoming more prevalent. It can even cause a blindness if used near the orbit. Interventional Neroradiology and Oculoplastics Surgery conducted a study to evaluate the vascular perfusion effects of topical nitroglycerin paste in an animal model using indocyanine green (ICG) imaging. (Investigators: )
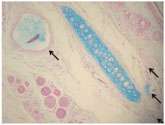
The soft tissue filler in the larger arteries and the smaller arterioles and capillaries (arrows).