Colorectal cancer is the second-leading cause of cancer deaths among men and women combined in the United States, yet it is estimated that 60 percent of those deaths are preventable through current screening methods.
Why, then, are people so hesitant to get screened?
"There's an 'ick' factor when it comes to colorectal cancer screening because people don't want to talk about" these issues, said Fola May, MD, PhD, a gastroenterologist at UCLA Health and an assistant professor in the Vatche and Tamar Manoukian Division of Digestive Diseases at the David Geffen School of Medicine at UCLA. "Making a point to talk about is the only way to make sure that people known about colon cancer risk and get screened."
The main screening methods are the colonoscopy and the fecal immunochemical test, or FIT, kit.
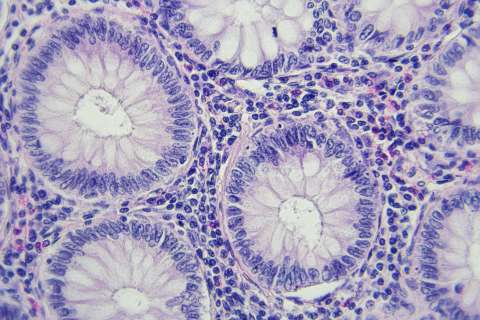
The colonoscopy, a 30-minute procedure that requires people to drink a colon prep the day earlier, is the most common method and is only performed once every 10 years if everything looks normal. If potentially-cancerous growths known as polyps are found during a colonoscopy, the gastroenterologist often can remove them during the procedure.
The FIT kit, a test in which the patient collects a small stool sample, is an alternative screening method that must be done annually. If blood is found in the sample, the doctor will recommend a colonoscopy for further observation.
Dr. May, also a member of the UCLA Jonsson Comprehensive Cancer Center, discussed some of the factors that make patients uncomfortable and may prevent them from getting screened.
For those who don’t want to get a colonoscopy, what are the alternatives?
Patients hesitant about colonoscopy can do a FIT kit at home. A lot of people think the stool collection process is messy or gross, but we provide a clean and easy way to collect the sample. About 7 to 10 percent of people who use a FIT kit receive a positive result – a confirmation of blood in the stool, which could indicate a cancer or a polyp – meaning they then have to get a colonoscopy anyway.
For the average person, we don't care which initial screening method you pick, as long as you choose one and prioritize getting it done.
What is the prep like? Is it really as awful to drink as I’ve heard?
Prior to a colonoscopy, people will have to drink a prep liquid the day before, which helps empty the colon so that we can clearly inspect the colon walls for polyps during the procedure. And yes, it is far from delicious. It can taste like salty water.
But think of it this way: most people only have to get a colonoscopy once every 10 years, which means you’re likely to only have to do the prep once every 10 years. This screening test can also find polyps and cancer early, which can save your life. So, it’s definitely worth drinking the prep.
If you can, plan not to do much on your prep day. This is the day that you get to turn on Netflix, chill out, and stay near your bathroom.
Will I be awake during the procedure?
We typically use monitored anesthesia care for our colonoscopy procedures at UCLA Health. Medications are administered to the patient through an IV and the patient is monitored by a qualified anesthesia provider. This anesthesia provider is focused exclusively on the patient’s airway and vital signs, while the gastroenterologist is allowed to focus completely on performing the colonoscopy. This puts you into a pain-free state during the procedure and allows for a quick recovery once the colonoscopy is done.
Everyone frets the actual procedure, but very few people actually remember it. Many patients wake up after the colonoscopy asking when we are going to get started!
Will the colonoscopy hurt?
No, it shouldn't. At most, you'll feel some pressure.
If you're feeling any pain, we'll typically give more medication. Our job is to make sure everyone is as comfortable as possible.
What's the difference between this and a prostate exam?
A lot of men are confused about the difference between a colonoscopy and a prostate exam.
Prostate cancer and colorectal cancer are conditions that typically occur – and must be screened for – in older age. The confusion seems to stem from the fact that screening methods for each involve an evaluation through the anus.
Getting screened for prostate cancer includes a digital rectal examination in which a doctor places a finger into the rectum for about five seconds to feel for an enlarged or abnormal prostate. Because the prostate is located next to the rectum, we can feel it by pressing on the back wall of the rectum.
In a colonoscopy, we use a tiny camera with a light on the end to examine the walls of the colon. The colon is six feet long, so a colonoscopy goes much further than a prostate examination. While they are completely different procedures, both are part of a healthy screening program for men as they age.
What if I accidentally pass gas during the procedure?
Patients are so worried about passing gas during the colonoscopy.
Guess what? You're going to. Everyone does. You won't be the first and won't be the last. And if you don't let the gas out during the procedure, you're going to feel pretty uncomfortable. We are able to examine the colon walls so well because we put air into the colon as we do the colonoscopy to distend the walls. We always encourage patients to let that gas come out naturally.