The COVID-19 pandemic could produce a devastating side effect felt for years to come – worse breast cancer outcomes.
Nationally, screenings for breast cancer plunged in the early months of the pandemic and have not yet returned to normal. The decline, coupled with treatment delays, have led some cancer experts to forecast an increase in deaths.
“There’s definitely the concern that the drop in screenings and the lack of return to normal screening rates can fuel a delay in diagnosis, which can lead to a later stage at diagnosis and potentially more deaths," said UCLA Health breast surgeon Deanna Attai, MD, FACS. “Some of it will depend on how quickly people get back to screening.”
Dr. Attai said some patients are worried about having a mammogram because of COVID-19 or have lost their health insurance, which would cover the test, in the economic fallout from the virus.
“The whole point of any screening test is to improve survival of the cancer, not just to detect it,” she said. “We know that, in general, the use of screening mammograms will result in improved outcomes from breast cancer.”
Starting in March, routine medical appointments were canceled to conserve resources for coronavirus patients and prevent further spread. Additionally, women who already had been diagnosed faced delays to surgery, chemotherapy or radiation, which could increase mortality rates, said Dr. Attai, an assistant clinical professor of surgery at the David Geffen School of Medicine at UCLA.
“There are many, many layers,” she said. “It’s not as simple as just screenings were shut down for a couple months.”
Even after appointments resumed, breast cancer screenings in mid-June were 29% lower than pre-pandemic volume, according to data from Epic, a medical records company.
In June, the director of the National Cancer Institute, Norman Sharpless, MD, wrote in the journal Science that a conservative model forecast nearly 10,000 excess deaths from breast and colon cancer in the next decade because of drops in screening and treatment. That amounts to an increase of roughly 1%, with deaths peaking in the next year or two.
Breast cancer screening guidelines differ, but generally asymptomatic women, starting between age 40 and 50, are advised to undergo a mammogram once a year or every other year until at least age 75. Annual screenings are recommended for women who have had breast cancer, or have a family history of breast cancer or certain genetic mutations that increase risk of developing breast cancer. Dr. Attai said the test can find suspicious lumps that are too small to feel.
For women whose appointments were canceled in the spring, a three-month postponement will generally not make a big difference in outcomes, Dr. Attai said. But some patients have said they won’t be screened until there’s a vaccine, which still could be many months away.
“Are these patients just not coming back because they’ve decided they’re not leaving the house for a year?” Dr. Attai said. “The question is are they lost to screenings at this point?”
Mammogram decision
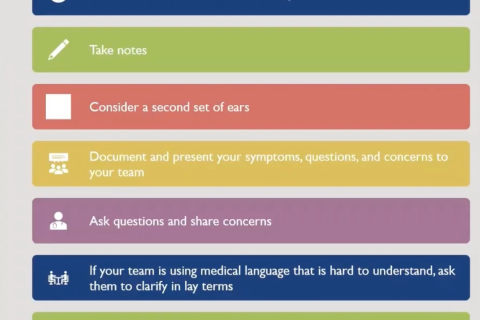
Dr. Attai said she’s counseled patients who are struggling to weigh the risks of potential coronavirus infection with their concern about skipping a cancer screening.
“This is a virulent virus. It’s contagious,” Dr. Attai said. “When you go in for a mammogram, it’s not a no-touch procedure. You’re in direct contact with the technologist who’s positioning you in the machine.”
She said for patients with anxiety, she’s advised them to contemplate their worst case scenario: Is that the possibility of contracting COVID-19 or postponing a mammogram and later finding cancer that could have potentially been diagnosed earlier?
The decision can be particularly difficult for women with a history of breast cancer, those with underlying conditions that put them at greater risk of serious illness from the coronavirus, or patients who are caring for elderly parents.
“It causes, obviously, a lot of worry,” she said. “The messaging over the years has been the importance of screening and early detection.”
Dr. Attai said women should discuss their risk factors for COVID-19 with their primary care doctors, who she said can also provide insight about the extent of infection in various parts of the county to help gauge the risk of booking a mammogram.
“I have some patients who are concerned that infection rates are going to pick up in the fall when flu season starts again, so they feel like there’s a little bit of a window right now,” Dr. Attai said.
She also advises patients to call their imaging facility in advance to ask about safety protocols. Dr. Attai told a nervous patient about her own experience getting a mammogram over the summer. Everyone wore a mask, many chairs had been removed from the waiting room to ensure physical distancing and a sign informed patients they could also choose to wait in their cars. The technician sanitized the testing equipment in her presence.
Economic pain
Dr. Attai said she’s particularly concerned about the crush of women who lost insurance coverage as unemployment skyrocketed. An analysis by the nonprofit Families USA estimated that 5.4 million workers lost health insurance during the first three months of the pandemic.
“I think that’s going to be the bigger problem – you found the lump, or you got your screening mammogram and it showed a suspicious finding,” Dr. Attai said. “Now how are you going to pay for the additional imaging, biopsy and treatment when you can’t afford your rent or your mortgage?”
Low-income and women of color already face inequities in screening and in breast cancer death rates. The Pew Research Center found that more women than men have lost their jobs this year. Black women and Latinas have been hit particularly hard.
“Loss of health insurance, financial instability and inability to pay for the diagnostic studies, the biopsy, and the subsequent cancer treatment certainly has the potential to have a major impact on cancer outcomes and survival rates,” Dr. Attai said. “There’s definitely the potential to exacerbate the health care disparities we already have.
Get more information on breast cancer through UCLA’s Jonsson Comprehensive Cancer Center.
Courtney Perkes is the author of this article.