Dear Doctors: I recently had a surgical procedure and was in the hospital for a few days. While I was there, I was diagnosed with pseudomonas. Can you please explain what that is? How do you get it? I was prescribed antibiotics, but it has not gotten rid of the infection. What happens next?
Dear Reader: Pseudomonas is a genus of bacteria that we encounter every day. It is found throughout the natural environment, including in soil, water and vegetation.
The genus encompasses several hundred different species, and it includes a handful that can cause infections in humans. Among these is a species known as Pseudomonas aeruginosa. Commonly shortened to P. aeruginosa, this bacterium has migrated into the built environment, including health care settings. It has been found on surfaces as diverse as floors, sinks, countertops, bed rails and medical equipment.
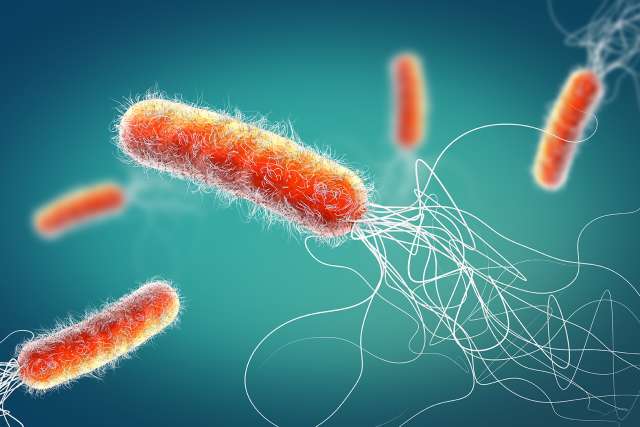
The bacterium is shaped like a rod, with a thin tail that propels it with a whiplike motion. It needs very little food or water to survive, and it can persist on surfaces for months. In one experiment, a species of pseudomonas was found to be able to survive for months in distilled water. This has led some scientists to refer it as the cockroach of the microbial world.
In the majority of healthy people, pseudomonas causes only mild symptoms. However, when it is acquired in a health care setting, it can become a more serious threat. It is estimated that infection with P. aeruginosa causes up to 20% of health care-acquired infections. With the ability of pseudomonas to survive in difficult conditions and to evade the effects of many available antibiotics, it's clear why the bacterium is widely viewed as a grave threat.
If pseudomonas is present on medical instruments, on the patient's or caregiver's skin, or in the environment, there is a risk that it can enter the body. This can be via the blood, the lungs and areas of the body where the skin has been breached. Each pathway can lead to infection.
People who have had surgery, are on a catheter or a breathing apparatus, are being treated for burn wounds or are undergoing intravenous therapies are at increased risk. So are those with impaired immunity, such as patients undergoing cancer treatment or organ transplantation and individuals living with immunodeficiency disorders.
Treatment for this type of infection typically begins with a test to ascertain whether the microbe is resistant to antibiotics. This is known as culturing. The results of the culture then serve as a guide for the specific classes and types of antibiotics that each patient will be prescribed.
Unfortunately, as has occurred in your case, it can take more than one attempt to arrive at a successful treatment. It is possible that your medical team will begin by repeating the culture procedure, then prescribe a different antibiotic regimen. This entails the use of multiple classes of antibiotics to overcome the defenses the bacterium has developed. It may also necessitate the use of increased dosages and longer treatment times. Depending on the site of the infection, the resulting symptoms are addressed as well.
(Send your questions to [email protected], or write: Ask the Doctors, c/o UCLA Health Sciences Media Relations, 10960 Wilshire Blvd., Suite 1955, Los Angeles, CA, 90024. Owing to the volume of mail, personal replies cannot be provided.)