UCLA Health has received certification from the U.S. Food and Drug Administration (FDA) to be among a select group of health systems across the nation to administer a new treatment for certain types of lymphoma and leukemia that genetically modifies a patient’s own cells to attack the cancer. Chimeric antigen receptor (CAR) T-cell therapy fights the cancer by redirecting T cells, which play a central role in the immune response, to enhance the body’s natural defenses.
Two CAR T-cell treatments have been approved by the FDA, and UCLA Health is among the few institutions providing such therapy outside of clinical trials — a setting in which UCLA has offered the treatment for several years. Dr. Josh Sasine, director of UCLA Health’s new CAR T-cell program, talks about the promising results the therapy has produced and the larger significance of the approach.
How does CAR T-cell therapy work?
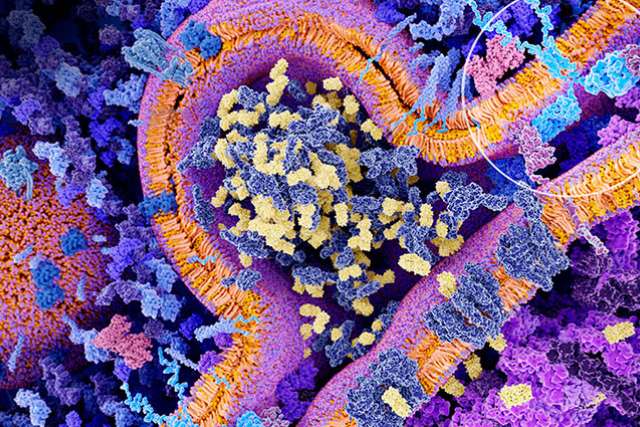
CAR T-cell therapy combines several approaches to cancer treatment: cell therapy (such as a bone marrow transplant), immune therapy and gene therapy. Healthy immune cells — specifically, T cells — are separated from a patient’s blood. Then, in the laboratory, manufacturers insert a chimeric antigen receptor, which is a synthetic gene that can recognize certain types of cancer cells. These genetically altered immune cells are grown in the lab to clinically relevant numbers and we reinfuse them into the patient. These T cells now have the ability to recognize and eradicate the cancer cells, much as they would in the case of an infection.
So, in a nutshell, it is an approach to strengthen the immune system’s ability to fight off the cancer?
Exactly. In this case, it’s a genetic modification doing the work that would normally be done naturally by the immune system. We have known the immune system is involved in protection from cancer for a long time. For example, if the immune system is suppressed, either after an organ transplant or because of a virus such as HIV, patients are at higher risk for developing cancers. So, we know that the immune system does clear out cancer naturally; this is the revved-up version of that.
Who is the therapy for?
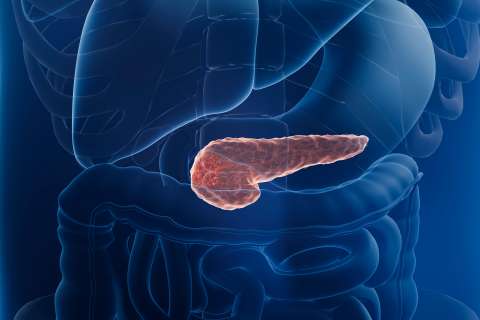
For now, this is only for patients with blood cancers that arise out of B cells, which are the cells that naturally produce antibodies. Most lymphomas in adults and leukemias in children arise from this population of cells. CAR T-cell therapy is only offered to patients with these cancers who have not benefited from two standard treatments. That’s because CAR T cells can overstimulate the immune system and cause inflammation, which can lead to significant side effects. However, the vast majority of patients with these cancers who have not benefited from at least two standard therapies will die within a year without CAR T cells. With them, their survival is above 50 percent.
Beyond those numbers, what is significant about this treatment?
The significance is twofold. One is that the degree to which some patients benefit is remarkable. Most successful therapies for advanced cancers increase overall survival by a few months but almost never cause long-term remissions. With CAR T cells, we’re seeing durations of benefit that are very long lasting — many years of cancer-free periods. About one-third to half of the patients who receive this therapy are having durable remissions. But the treatment is so new that we don’t yet know who has experienced a true cure. It also is significant that this treatment platform is very different from what we have done in oncology in the past, and, in principle, it is broadly applicable. Until ongoing and future clinical trials are complete, we won’t know whether or not we can make CAR T cells recognize other forms of cancer. If we can, this could benefit many more patients.
Do you expect to see this approach tested in many other cancers?
Testing for other cancers is currently ongoing. It is one thing to have success in the lab, but the fact that we are seeing so much success with CAR T cells validates the idea that we can genetically engineer the immune system to fight cancer. This is likely to encourage investigators to examine other strategies to genetically engineer immune cells for cancer therapy. It opens up an exciting new direction. I have not seen any other approach demonstrate this much success so quickly.