A personalized vaccine developed by UCLA Health scientists has been shown to potentially extend the life of patients with glioblastoma, the most aggressive form of brain cancer.
As the therapy awaits submission for approval to the U.S. Food and Drug Administration, it is one of the latest examples of UCLA Health research moving from the bench to the bedside.
The results of two other clinical trials at UCLA could also soon provide new therapy options for patients with Alzheimer’s — a disease for which there is no cure and few treatments to manage symptoms. The FDA has granted “accelerated approval” for the amyloid-targeting drug lecanemab, which has been shown to moderately slow cognitive decline.
A similar drug, donanemab, showed promise in a phase 3 study.
“An institution like UCLA offers patients with progressive and ultimately life-ending diseases the opportunity to participate in trials that may benefit them, but the primary goal of any clinical trial is to provide benefit to others,” says S. Thomas Carmichael, MD, PhD, chair of the Department of Neurology at the David Geffen School of Medicine. “When the FDA approves a new therapy, that benefit becomes a reality.”
A vaccine to treat glioblastoma
Glioblastoma is the most aggressive primary brain tumor in adults, with more than 10,000 new cases diagnosed in the United States each year. Standard treatment involves surgery, radiation, and chemotherapy; and the median overall survival rate is only 15 to 17 months from diagnosis.
A vaccine to treat glioblastoma called DCVax-L has been in development for several years. Linda Liau, MD, PhD, MBA, and a team of UCLA researchers were the first to investigate whether a patient’s own dendritic cells (a specialized type of immune cell) could be used to create a personalized treatment for the deadly cancer.
“We tested the method with a single patient in 1997, and then moved to a phase 1 safety trial in the early 2000s,” says Dr. Liau, professor and chair of Neurosurgery at UCLA.
A series of phase 2 early efficacy and optimization trials followed, and then an international, multi-site study led by Dr. Liau began in 2007.
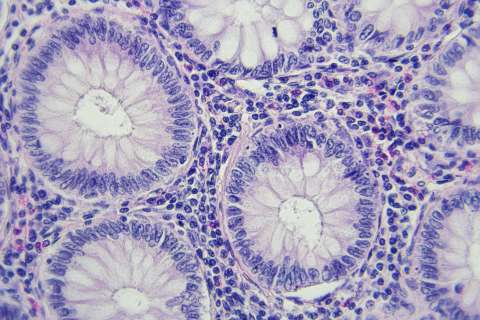
The vaccine consists of two components: a patient’s dendritic cells, which are special types of immune cells, and proteins prepared from a patient’s tumor.
To create the vaccine, which is individualized for each patient, medical staff first perform a procedure called leukapheresis, in which a patient’s blood is drawn and their white blood cells are collected. Then, the patient’s tumor is removed and sent to a lab where researchers obtain proteins from the specimen, called tumor lysate. The white blood cells are cultured to differentiate into dendritic cells, and then combined with the tumor lysate to make the vaccine.
Dendritic cells are “antigen-presenting” cells, which means that they are able to process all kinds of foreign invaders in the body and alert the immune system’s T cells to mobilize a broad immune response against those invaders. Glioblastoma is a highly heterogenous disease, meaning there are many different types of cancer cells within a single tumor. Therefore, the dendritic cells — loaded with a patient’s own tumor lysate — allow a patient’s immune system to recognize a wide variety of tumor targets and spur the immune system to respond, according to Dr. Liau.
The phase 3 trial led by Dr. Liau involved 331 study participants at 80 sites around the world from August 2007 to November 2015. During the study, 232 people received standard care and DCVax-L at new diagnosis, while 64 out of 99 people received standard care and a placebo. (Patients in the placebo group received the DCVax-L at recurrence.)
The trial results, published in JAMA Oncology in November 2022, showed that newly diagnosed glioblastoma patients receiving the vaccine had an overall survival of 19.3 months on average, compared to 16.5 months on average among the contemporaneous, matched external control group.
“There is a significant subgroup of patients who lived more than five years, but the challenge is trying to determine which patients it may work for, and for which patients it doesn’t,” Dr. Liau says.
At UCLA, Dr. Liau and other researchers are now testing whether the vaccine would be more effective in combination with a PD-1 checkpoint inhibitor. Checkpoint inhibitors are a type of immunotherapy that work by blocking proteins that stop the immune system from attacking cancer cells. While the vaccine allows T-cells to get inside of the tumor, the checkpoint inhibitors may allow T-cells to be more functional and better attack the tumor cells.
“Because of the heterogeneity of glioblastoma, I don’t think there is going to be one drug or one treatment that is going to be effective for all patients. The future of glioblastoma treatments is going to be these combination approaches,” Dr. Liau says.
Hope for an Alzheimer’s cure
The diagnosis of Alzheimer’s disease, which is rapidly increasing in prevalence and incidence worldwide, can lead to a sense of “hopelessness” among patients, their caregivers, and their doctors, says Dr. Carmichael.
More than 6 million Americans have the disease — the sixth leading cause of death in the United States.
“There is even a sense of nihilism in doctors, who think, ‘Well, if a patient has memory loss, why even test them for Alzheimer’s?’ Because whether they have the disease or another kind of dementia, we can’t do much to help them.”
Following years of failed — and some controversial — trials for Alzheimer’s therapies, one drug will soon be available to patients, with another on its way.
The treatment lecanemab was granted accelerated approval by the FDA in January of this year. The drug, sold under the brand name Leqembi, is made by the pharmaceutical company Eisai in partnership with Biogen, and is delivered to patients by an intravenous infusion every two weeks.
The drug targets the sticky, abnormal protein amyloid, which builds up in the brain and is a hallmark of Alzheimer’s. Participants who received lecanemab in the phase 3 clinical trial showed a significant reduction in amyloid in imaging tests. However, the reduction in amyloid did not necessarily translate to dramatic cognitive improvement. The results from the multi-site clinical trial were published in the New England Journal of Medicine.
Lecanemab also comes with a high price tag, and access to the drug will depend on whether it receives traditional FDA approval and could be covered by Medicare.
Lilly has applied for FDA approval of its Alzheimer’s drug, donanemab, which similarly targets amyloid. Results from its phase 3 trial have not been peer-reviewed, but a press release from the pharmaceutical company said that nearly half of participants had no clinical progression after one year.
“What’s been surprising, and a bit disappointing, is that these drugs didn’t have as dramatic an effect on cognitive recovery or cognitive decline,” Dr. Carmichael says. “They had a very, very — that’s two ‘verys’ — modest effect on cognition.”
Still, even a modest effect on cognition is notable for patients living with an incurable, degenerative disease, Dr. Carmichael says. And, most importantly, it opens the idea that Alzheimer’s is indeed treatable.
“The scientific community has essentially finished with amyloid — we’ve identified it, developed drugs, and can clear it,” Dr. Carmichael says. “The fact that clearing amyloid doesn’t substantially change the progression of the disease means that other things are also going on in the brains of Alzheimer’s disease patients.”
At UCLA, researchers are investigating, for example, how inflammation may impact Alzheimer’s disease progression, as well as the role of the protein tau.
“There are a lot of interesting questions,” Dr. Carmichael says, “that now are even more important to answer.”
Lauren Ingeno is the author of this article.