Dear Doctors: Our daughter is 24 years old. She struggled with her health for several years before finally being diagnosed with lupus. I’m reading as much as possible about this disease and have seen a study with a potential cure called CAR T-cell therapy. What is it, and how does it work?
Dear Reader: For those who aren’t familiar, lupus is an autoimmune disease. That means the immune system mistakenly identifies the body’s own tissues as foreign invaders and attacks them. This results in damaging inflammation that, over time, leads to a wide range of symptoms. These can include fatigue, fever, stiffness or pain in the joints or muscles, skin problems, sensitivity to sunlight, headache, dry eyes, hair loss and mouth sores. Lupus can also cause damage to the internal organs, particularly the lungs and kidneys. It can also affect the nervous system and the heart. There is no known cure at this time.
Treatment for lupus involves the use of medications to reduce inflammation and manage symptoms, and to prevent organ damage. Now, as you have read, research into something known as CAR T-cell therapy in lupus patients has shown promise. Unlike traditional lupus treatments, which can only ease the effects of the disease, CAR T-cell therapy hints at a path to remission. And while the research that you read about produced good results, it’s important to understand it’s not yet a breakthrough. The study in question was quite small, with just five patients. Neither the long-term success of this new approach, nor its potential long-term side effects, are yet known.
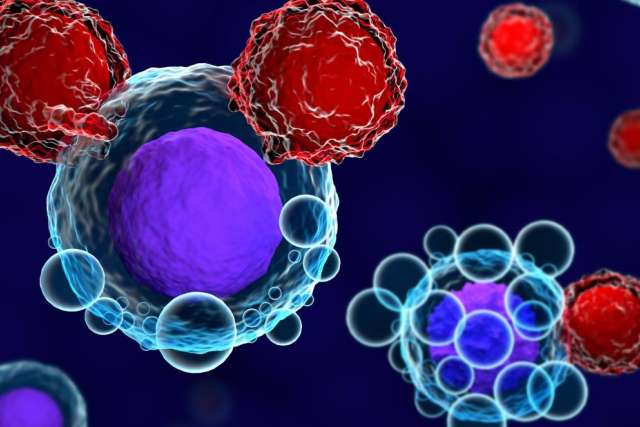
CAR T-cell therapy is a type of immunotherapy. These are treatments that harness the behaviors and activity of certain immune cells to fight disease. Five years ago, the FDA began to approve CAR T-cell therapy for use in some blood cancers. As the name suggests, this treatment uses T cells, which are a type of white blood cell. The first step is to collect blood from the patient and extract the T cells. These are then genetically modified so they will act upon a specific target. For the lupus study, researchers “taught” the CAR T cells to target the overactive immune cells that attack the body’s own tissues. Up to 100 million CAR T cells were needed for a single therapeutic dose, so the customized cells were reproduced in the lab. Each patient was then infused with their own customized cells.
About three months later, after the CAR T cells had eliminated the malfunctioning immune cells, the patients' bodies began to produce new immune cells, all of which behaved normally. Each of the five patients in the study has been able to stop taking the drugs that were being used to manage their illness, and they are considered to be in remission. But -- and it’s an important “but” -- the follow-up period at this time is less than two years. That, combined with the tiny sample size, keeps this treatment firmly in the realm of investigation. More study, with more patients and ongoing follow-up, are needed for CAR T-cell therapy to be effectively evaluated as a potential treatment for lupus.
(Send your questions to [email protected], or write: Ask the Doctors, c/o UCLA Health Sciences Media Relations, 10960 Wilshire Blvd., Suite 1955, Los Angeles, CA, 90024. Owing to the volume of mail, personal replies cannot be provided.)