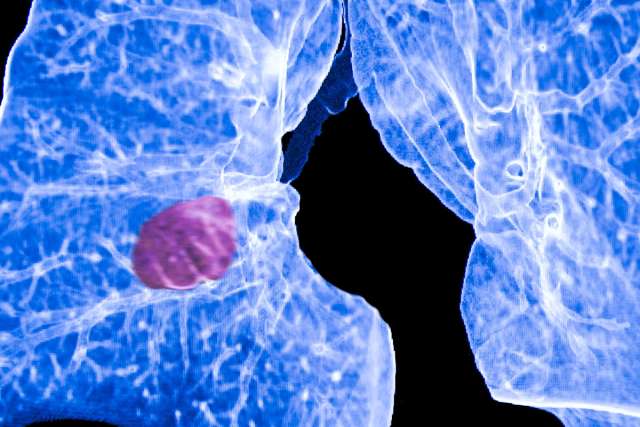
Researchers at UCLA’s Jonsson Comprehensive Cancer Center, on a quest to find lung cancer stem cells, have developed a unique model to allow further investigation into the cells that many believe may be at the root of all lung cancers.
If researchers could find a way to isolate and grow lung cancer stem cells, they could study their biologic mechanisms and perhaps identify targets for new therapies, said Raj Batra, an associate professor of medicine and a Jonsson Cancer Center scientist.
“What this model allows us to do is test, in patient specimens, which markers indicate the presence of lung cancer stem cells,” said Batra, senior author of the study. “Our ultimate goal is to define lung cancer and the cells that cause it so we can develop more effective therapies.”
The study appears in the June issue of PLoS One, a peer-reviewed journal of the Public Library of Science.
Two competing theories of how cancer originates have been weighed by scientists for decades. In one theory, all the cells of a tumor are the same, with an equal capacity to divide and form new tumors. The other theory holds that only a few, select cells from a tumor have the ability to initiate a new tumor — the cancer stem cells. In the last decade, scientists have been able to isolate leukemia stem cells as well as brain and breast cancer stem cells. Many scientists believe that most, if not all, cancers will one day be traced back to these stem cells.
Only a small percentage of cells in a tumor are cancer stem cells, making them hard to find and even more difficult to target. Current cancer therapies are designed to target dividing cells, and the treatments do kill the majority of the cancer cells. But cancer stem cells can lay dormant and survive chemotherapy as well as the molecularly targeted treatments now being used. Because they’re not actively dividing, they’re invisible to conventional treatment methods.
At some point, the cancer stem cells begin their process of self-renewal and differentiation, creating a new tumor. This explains why people can remain cancer free for years and still suffer a recurrence.
Lung cancer, Batra said, is not a single disease but a collection of sub-types with different characteristics. Some lung cancers are invasive and spread quickly throughout the body, while some become drug-resistant. There may be a single lung cancer stem cell causing the different sub-types, or there may be a different lung cancer stem cell responsible for each. Since cancer stem cells are known to possess unique properties — a predisposition to metastasize and to be drug-resistant — Batra has proposed to extract candidate cancer stem cells directly from clinical specimens based on the markers they express, and then validate these cells functionally.
In an effort to find lung cancer stem cells, Batra and his team collected specimens from patients with malignant pleural effusions, a condition in which an abnormal amount of fluid collects between the thin layers of tissue lining the outside of the lung and the wall of the chest cavity.
They had found in previous attempts that culturing lung cancer cells from tumors in Petri dishes did not work well. The cells that grew were not representative of the heterogeneous cells found in a tumor. Batra and his team sought to grow cells in an environment that was as close to that in which the tumor grows as possible.
By using the fluid from the pleural effusions, Batra hoped to be able to create a microenvironment in which the tumor cells would remain heterogeneous and enable researchers to more easily identify candidate cancer stem cells.
“Using the same environment the tumors were extracted from allows us to grow a much broader variety of tumor cells,” Batra said. “There’s much more heterogeneity.”
To provide proof of concept, Batra looked for both cell surface and epigenetic markers associated with cancer stem cells and found signatures for most of those markers in the cells they grew.
“We were able to establish cultures in vitro with high efficiency using the novel strategy that utilized an autologous tumor microenvironment,” the study states. “In this primary culture model, we have been able to provide proof-of-concept that candidate lung cancer stem cells are present, that candidate lung cancer stem cells can be maintained over time in this environment, and we can live sort candidate lung cancer stem cells from these primary cultures to evaluate their phenotype in various bioassays.”
Batra and his team were successful seven out of seven times in growing heterogeneous cell cultures from seven different patient specimens. Each of the seven specimens had molecular features indicative of cancer stem cells.
“We feel we were able to do this because we used not just the tumor cells but also the cells that accompany the tumor cells and the fluid they are living and growing in,” Batra said. “This will allow us to develop a more representative model of lung cancer.”
Judith C. Gasson, Jonsson Cancer Center director, said understanding lung cancer stem cells could lead to novel therapies that will better fight this disease, which kills more than 160,000 Americans every year.
“Jonsson Cancer Center researchers have been at the forefront of developing the current wave of targeted therapies that have been so successful in fighting cancer. But those treatments don’t reach the cancer stem cells,” Gasson said. “We need to understand the biology of the cancer stem cell so we can develop the next new wave of molecularly targeted therapies that go after those important cells.”
The four-year study was funded by Veterans Affairs Biomedical Research Funds.
Researchers Develop Model that May Help Identify Lung Cancer Stem Cells
Share:


