Breast milk feeding is perhaps the most natural and fundamental way for a newborn human being to begin their life in this world.
But that does not mean it always comes easily.
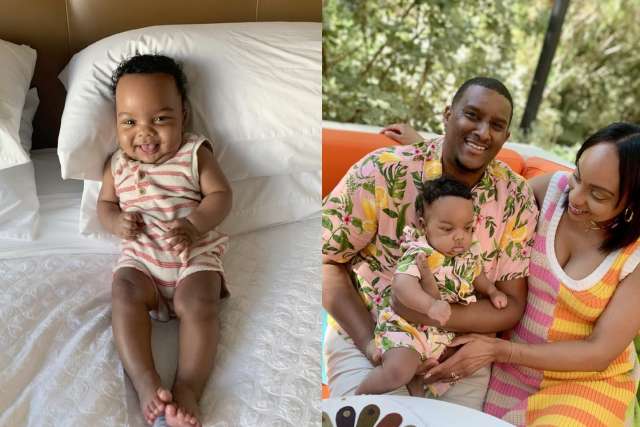
When Karina Dixon fulfilled her dream and had her first baby, a boy she named Zen, almost nothing went according to her carefully thought-out plans. Little Zen was born premature at 28 weeks, weighing only 3 pounds.
Experts at the UCLA Health Neonatal Intensive Care Unit (NICU) told the new mother that the most important thing she could do for her son was to breastfeed him as much as possible, to help him catch up in weight and development. But Dixon soon found that was much more easily said than done. Little Zen could not properly latch on, and he had difficulty feeding.
By pumping her breast milk and supplementing with pasteurized human donor milk and formula, Dixon was able to feed Zen, first by tube and then by bottle, for the 54 days he was in the NICU. Her baby boy was 6 pounds when she finally took him home.
Lactation consultants in the hospital aim to meet NICU families, such as Dixon and her son, as soon as possible. They teach hand expression and educate new parents on how to use a breast pump to safely collect, store and transport milk to their babies.
When babies are in the NICU hand expression and pumping of breast milk, skin-on-skin contact with baby, and performing oral care with swabs of the birthing parent’s colostrum are a few ways to help build milk supply and promote bonding. Colostrum, a precursor to mature milk, is especially beneficial for fragile babies because it protects against infection.
Lactation consultants provided Dixon and Zen support in the NICU every step of the way before discharge. But at home Mom was worried about not being able keep her milk supply up and provide the best possible nutrition for Zen’s development.
"I got this feeling like I was never going to be able to breastfeed my baby. I got that anxiety into my head when it wasn't working, and stressed myself out about it, and I think that affected my milk production," she said. "When I was planning everything out, I imagined our breastfeeding journey to come naturally and didn’t imagine the need for outside support. I had no idea how hard it would be, and I felt really defeated."
Everything turned around when Dixon first visited the UCLA outpatient lactation program near her home in Santa Monica, on the advice of the NICU staff.
"From our first appointment with the lactation consultant, she could tell I was tense. But they were very positive and made the goal of exclusively breastfeeding seem more attainable by helping us to focus on little milestones to mark success. Our first priority was getting him to latch on, and once we did that, I started to feel like this really was going to work out," Dixon said. "We were able to celebrate these little successes along the way. So, then I was able to relax, and Zen and I could actually enjoy this process."
Things only got better for Dixon and Zen.
"They helped keep me relaxed, and I think breastfeeding actually stimulated my milk production, so then I got to the point where I could supply all of my baby’s needs with breast milk,” Dixon said. “That's when everything finally came together, and I knew this was a success."
The UCLA Health lactation team strives to support all families with their infant feeding goals. International Board Certified Lactation Consultants (IBCLCs) are available every step of the way – from prenatal lactation consultations, to in-hospital support, from in-person one-on-one appointments, to virtual and in-person support groups.
Tina Daunt is the author of this article.