When Shaunté Walton, MS, CIC, and her team of infection preventionists at UCLA Health first became aware of Candida auris causing significant outbreaks in the U.S. in 2019, they jumped into action to prevent its spread before the first case reached Los Angeles County.
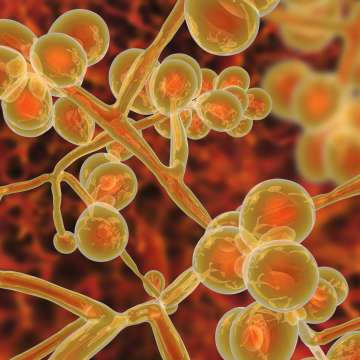
Candida auris (commonly known as C. auris) is an exceptionally virulent hospital-acquired fungal infection that is often resistant to antifungal drugs and can lead to severe illness in hospitalized patients. In some patients, the pathogen can enter the bloodstream and spread throughout the body, causing serious bloodstream infections, wound infections and ear infections.
There has been a recent uptick in C. auris cases in U.S. hospitals and nursing homes. In 2022, the Centers for Disease Control and Prevention recorded more than 8,100 infections – a nearly 50% increase over the 5,500 recorded in 2021. According to the CDC, one in three people who contract the pathogen will die.
Walton, system director of Clinical Epidemiology and Infection Prevention at UCLA Health, notes that C. auris is exceptionally dangerous for immunocompromised individuals and those who have been hospitalized for an extended period of time. Individuals who have a central venous catheter or other lines or tubes entering their body also are at high risk, as these invasive devices open a path for the fungus to enter the body.
Partnership with IT
Early on, Walton and her team partnered with UCLA Health’s Information Technology Systems to create a risk assessment tool that screens every patient who enters the hospital, whether they come in as a direct admit or through the emergency department.
The risk assessment asks a series of questions related to high-risk criteria as determined by the CDC and the Los Angeles County Department of Public Health.
"High-risk patients include, but are not limited to, those admitted from a facility identified to previously have a C. auris outbreak, those who are on a ventilator or who have a tracheostomy, those who have a history of CRE (antibody-resistant bacteria), or those who have been admitted to an acute-care hospital outside of California or outside of the U.S.," says Urvashi Parti, an infection preventionist on Walton's team.
UCLA Health’s lab is able to test for C. auris in-house, Parti says.
“If the patient meets the screening criteria for high risk, we are able to collect a swab,” Parti said. “This is active surveillance testing, which allows for early identification of C. auris, which helps prevent potential outbreaks.”
If a patient tests positive for C. auris, the patient’s infection status is flagged in their electronic record and will remain there forever, even after discharge.
“This helps isolate and protect the community,” Parti says.
Positive-status patients are managed in contact isolation, meaning health care workers must wear gowns and gloves and use a sporicidal, hospital-approved disinfectant to clean and sanitize the patient’s room. UCLA Health’s Environmental Services team is notified so they can oversee the management of the room once the patient is discharged.
Not a new fungus
C. auris was first identified in Japan in 2009, but, in retrospect, the earliest known strain is believed to have originated in South Korea in 1996. The first case reported in the U.S. was in 2013. C. auris first appeared on Walton’s radar when she learned about the havoc it was creating at other health care facilities, where outbreaks forced hospitals to remove pipes and drains and take down ceiling tiles and flooring to rid it from the environment.
"Public health officials continue to heighten awareness among health care professionals about the dangers of C. auris," Walton says. "It's very hardy, and it persists in the environment for several weeks."
UCLA Health’s electronic records system was crucial to preventing an outbreak when 11 patients tested positive in 2021, she told the Washington Post recently.
Because the system was implemented early, there have been no clusters or outbreaks at UCLA Health, she says, “which indicates our protocols are working.”
She notes that the manual processes many hospitals have implemented to manage C. auris have led to challenges in communications.
“I think we’re one of the unique health care systems that utilized their electronic system to manage this pathogen effectively,” Walton says.
Jennifer Karmarkar is the author of this article.



