Nephro-Genetics

What should I know if I have a family history of chronic kidney disease (CKD) or other kidney-related problems?
Patients with family members who have been affected with kidney disease or related health issues should consult with a healthcare professional and see if they need to be screened for kidney disease. This is especially important for those with a family history of the following conditions:
- Diabetes
- Hypertension
- Heart Disease
- Kidney Infection
- Kidney Stones
- Prostate Disease
- Obesity
- Abnormal Kidney Structure
You are at increased risk if you are of African-American, Native American, or Asian-American descent.
How can I decrease my risk of developing chronic kidney disease, in spite of my family history
Use over-the-counter medications like pain relievers as directed. Misuse may lead to kidney damage, and a healthcare professional should be consulted before use should any concerns arise.
Stay physically active. Maintaining weight that is healthy for you is important in reducing risk for development of CKD.
Do not smoke. Smoking can further damage your kidneys. Seek out counseling or other forms of support to stop.
Keep your doctor (or some other healthcare professional) informed. If your primary care physician is frequently updated as to your health, physical activity, and other lifestyle choices, they will be able to better assist you in reducing risk of kidney damage and chronic kidney disease.
What about polycystic kidney disease?
Autosomal Dominant Polycystic Kidney Disease (ADPKD)
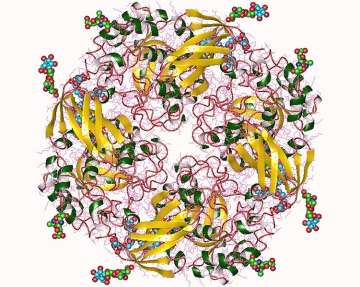
ADPKD is caused by a mutation in one of two genes, PKD1 and PKD2, which code for the proteins polycystin 1 and polycystin 2. These mutations lead to the formation of fluid-filled cysts on the kidneys, which damages and scars the kidneys. This condition can present as kidney failure, high blood pressure, or as a kidney infection.
Because ADPKD is an autosomal dominant disease, it can be caused by a mutation in just one of the two copies of the gene in an individual. Since only one copy is needed, it is likely that one of the parents of an affected individual also had the disease, and their children may also inherit the disease.
Autosomal Recessive Polycystic Kidney Disease (ARPKD)
ARPKD is caused by a mutation in the PKHD1 gene, which codes for the protein fibrocystin. Like ADPKD, ARPKD involves the formation of fluid-filled cysts on the kidneys. It also affects organs besides the kidney, including the liver.
Genetic testing can be useful for the diagnosis of ARPKD, since it can confirm the presence of a mutation in the PKHD1 gene. Since there are other diseases that can present similarly in newborns and some milder forms of the disease do not show up until later in childhood, this confirmation can help make a more definitive diagnosis.
Genetics in Alport Syndrome
X-Linked Alport Syndrome (XLAS)
X-Linked Alport Syndrome is the most common documented form of Alport Syndrome and it is caused by mutations in the COL4A5 gene, which is located on the X-chromosome. Females with XLAS are less affected than males because females have two copies of the X-chromosomes and males only have one copy, along with a Y-chromosome.
Females with XLAS have two copies of the COL4A5 gene, one copy of the gene carries the mutation, and the other copy of the gene is normal. The normal copy of the gene masks the effects of Alport Syndrome, which is why girls with XLAS have milder symptoms than boys. Males don’t have that normal copy of the gene to mask the effects like females have, therefore, they are almost always affected severely and eventually develop kidney failure at some point in their lives. However, females with XLAS can still develop kidney failure.
Males have one X-chromosome and one Y-chromosome, so males with XLAS will always pass down their affected X-chromosome gene to their daughters, but they cannot pass it down to their sons. A female with XLAS has a 50% chance of having an affected child as they can pass down their affected X-chromosome.
Autosomal Recessive Alport Syndrome (ARAS)
Autosomal recessive Alport Syndrome is when both copies of a gene are defective. Autosomal Recessive disorders happen when each parent of a child with a recessive condition passes down a mutant gene.
Autosomal Recessive Alport Syndrome is caused by mutations in the genes COL4A3 and COL4A4, which are located on chromosome 2. An individual with ARAS has two copies of the COL4A3 and COL4A4 genes. Parents have only one mutation in one of the chromosomes and so they can either show no symptoms or can have some hematuria (blood in the urine). A parent that carries a mutation in COL4A3 or COL4A4 has a 25% chance of having an affected child. Both males and females are equally affected with ARAS.
What is Fabry's Disease?
Fabry disease is a rare X-linked disorder, in which there is a deficiency of the ?-galactosidase A (α-Gal A) enzyme, making it a lysosomal storage disease. The deficiency is caused by mutations in the GLA gene. The lack of α-Gal A leads to a buildup of toxic materials, such as glycosphingolipids, specifically GL3 or Gb3, within the cells of the body. The buildup causes cell abnormalities and dysfunction of blood vessels, the heart, and the kidneys.
What are the current available standard treatments?
One current standard treatment is enzyme replacement therapy, which addresses the deficiency of the ?-gal A enzyme caused by mutations in the GLA gene. The treatment entails transfusions every two weeks for life; it is therefore not a permanent solution as it does not resolve the root issue of the mutated gene.
Another standard treatment is chaperone therapy, a molecular therapeutic approach targeted toward protein misfolding diseases. Migalastat is an orally-administered pharmacological chaperone that stabilizes mutant α-Gal A; in turn, the corrected forms of α-Gal A are delivered to the lysosomes, which promotes breakdown of excess Gb3, lysosomal trafficking, and enzyme activity.
What are some experimental treatments that are currently being researched?
Gene therapy is currently being researched as a viable treatment for Fabry disease. Gene therapy introduces a healthy copy of the GLA gene, which will produce the ?-gal A enzyme that was previously lacking. This is a relatively new treatment, so it is unknown if it is a one-time treatment for life or if other treatments will be necessary long-term. Additionally, there may be unknown side effects.
Another currently experimental treatment is substrate reduction therapy, which decreases the substrate level in order to balance the effect of the deficient enzyme. This in turn limits glycosphingolipid buildup.
Are there any potential candidates for gene therapy that might be used in the future?
One candidate for gene therapy in Fabry disease is known as AVR-RD-01. This is a single-infusion treatment that utilizes autologous lentivirus-transduced, CD34+-selected, hematopoietic stem/progenitor cells to express α-Gal A. It is currently being tested in clinical trials, and recent data shows consistent efficacy, as patients have experienced stable kidney function, as opposed to the declining function in typical Fabry disease sufferers.
Another candidate for gene therapy is FLT190. This uses a harmless virus to introduce a healthy copy of the GLA gene. It remains to be seen whether one or multiple infusions would be required, and this candidate is now being tested in a Phase ½ clinical trial for adult males.
One other candidate for gene therapy is ST-920. It has been deemed safe in a mouse model, which supported development of a clinical trial in humans. Current trials test the safety and efficacy of ascending doses of a single infusion of this therapy.
Webinars
Sources:
Fabry Disease. (2019, June 06). Retrieved May 25, 2021, from https://rarediseases.org/rare-diseases/fabry-disease/
Germain, D. P., Nicholls, K., Giugliani, R., Bichet, D. G., Hughes, D. A., Barisoni, L. M., Colvin, R. B., Jennette, J. C., Skuban, N., Castelli, J. P., Benjamin, E., Barth, J. A., & Viereck, C. (2019). Efficacy of the pharmacologic chaperone migalastat in a subset of male patients with the classic phenotype of Fabry disease and migalastat-amenable variants: data from the phase 3 randomized, multicenter, double-blind clinical trial and extension study. Genetics in Medicine, 21(9), 1987–1997. https://doi.org/10.1038/s41436-019-0451-z
Khan, A., Barber, D. L., Huang, J., Rupar, C. A., Rip, J. W., Auray-Blais, C., Boutin, M., O’Hoski, P., Gargulak, K., McKillop, W. M., Fraser, G., Wasim, S., LeMoine, K., Jelinski, S., Chaudhry, A., Prokopishyn, N., Morel, C. F., Couban, S., Duggan, P. R., … Medin, J. A. (2021). Lentivirus-mediated gene therapy for Fabry disease. Nature Communications, 12(1). https://doi.org/10.1038/s41467-021-21371-5
Moyses, C. (2003). Substrate reduction therapy: clinical evaluation in type 1 Gaucher disease. Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences, 358(1433), 955–960. https://doi.org/10.1098/rstb.2003.1271
National Kidney Foundation. Genetics and Kidney Disease [Internet]. New York (NY): National Kidney Foundation: 12 Aug 2014 [cited 13 Jul 2021]. Available from: https://www.kidney.org/news/kidneyCare/winter10/Genetics.
Suzuki, Y. (2014). Emerging novel concept of chaperone therapies for protein misfolding diseases. Proceedings of the Japan Academy, Series B, 90(5), 145–162. https://doi.org/10.2183/pjab.90.145
Tan, V. (2020, December 28). Gene Therapy for Fabry Disease. Retrieved May 25, 2021, from https://fabrydiseasenews.com/gene-therapy-for-fabry-disease/
University of Michigan Health: Michigan Medicine. Inherited Kidney Conditions [Internet]. Ann Arbor (MI): University of Michigan Health: [cited 13 Jul 2021]. Available from: https://www.uofmhealth.org/conditions-treatments/kidney/inherited-kidney-conditions.
University of North Carolina, Kidney Center. Genetics & Kidney Disease [Internet]. Chapel Hill (NC): University of North Carolina School of Medicine: [cited 2021 Jul 13]. Available from: https://unckidneycenter.org/kidneyhealthlibrary/genetics-kidney-disease-1/.
Walker, M. (2018, April 03). Enzyme Replacement Therapy for Fabry Disease. Retrieved May 25, 2021, from https://fabrydiseasenews.com/enzyme-replacement-therapy-for-fabry-disease/
Contributed by: Hannah Johnson-Stenger, Antony Lin, Tara Marashi, and Harshita Talkad (in association with Bruin Beans Health Club of the CORE Kidney Health Program)
Associated Faculty:
Bianca E. Russell, MD, FAAP, FACMG
Assistant Clinical Professor
Associate Program Director, Genetics Training Program
Division of Pediatric Genetics
Department of Pediatrics
University of California, Los Angeles
Marina Dutra-Clarke, MS, CGC
Licensed Certified Genetic Counselor
UCLA Institute for Precision Health
Division of Genetics
Department of Pediatrics
University of California, Los Angeles
Patricia L. Weng, MD
Pediatrics - NephrologyUniversity of California, Los Angeles