Brachytherapy at UCLA
The UCLA Brachytherapy Division is one of the most experienced and advanced centers in the United States. It was established in 2010 after D. Jeffrey Demanes was recruited to UCLA and brought his longstanding practice California Endocurietherapy to Los Angeles from Northern California.
We are one of the few centers in the United States that has expertise in using brachytherapy to treat all types of cancers.
We also have state of the art equipment and facilities including a brachytherapy suite in the Department of Radiation Oncology, a portable CT scanner to allow for imaging during implants, real-time ultrasound planning for prostate brachytherapy, a new Flexitron afterloader and a Xoft unit for intra-operative breast radiation.
Brachytherapy is a specialized skill and we’ve dedicated ourselves to building a team to take the best care of our patients as possible. Our team includes two nurses, a physician assistant, brachytherapy fellows, a dosimetrist, a physicist, two therapists, scrub techs, and front office staff. There are few other Brachytherapy centers in the United States that commit this level of resource to caring for brachytherapy patients.
History of Brachytherapy
Brachytherapyis a form of internal radiation treatment where radioactive sources are placed on or into cancer tissues. Sometimes the radiation is put in place through a larger metal or plastic tube called an applicator.
During the treatment, implants are placed in the body through the applicators. Some implants are permanent, while others are left in for a short period. The applicator may be removed at the same time as the implant, or it may be left in place until all the treatments are finished. Applicators can be placed either during surgery or by your physician using an imaging test to view the intended location. If the applicators need to be held in place, stitches may be used.
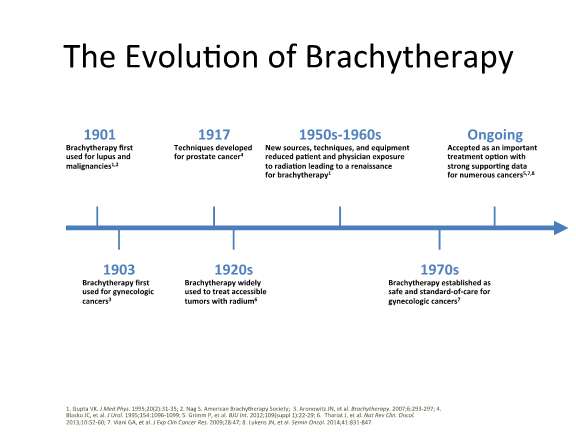
This is not a new technique. It has actually been around for over 100 years as can be seen in the below timeline:
Implant Types
Specific implants are selected based on the location of the tumor, the extent of the tumor, and several other factors. These types are:
- Intracavitary Implant: an applicator is inserted into a body cavity to reach the tumor. Intracavitary implants are performed in the UCLA Brachytherapy Suite on an outpatient basis.
- Intraluminal Implant: the catheters are inserted into a "tube" structure such as the bronchus, esophagus, or bile duct. These are also performed on an outpatient basis.
- Interstitial implant: are more complex. The implants are done in the operating room with the patient under local, general or spinal anesthesia. Interstitial catheters are inserted through the body tissue to encompass the tumor.
Brachytherapy Types
Low Dose Rate (LDR) Implants
LDR was once the only type of brachytherapy available. In this type of brachytherapy, the source of radiation stays in place for one to seven days. Most patients are hospitalized for the duration of this treatment, and once the treatment is completed, the radiation source is removed.
High Dose Rate (HDR) Implants
During HDR brachytherapy, the radiation source is in place for 10 to 20 minute periods and then removed. Depending on cancer type, HDR treatments may occur once or twice a day for two to five days or once a week for two to five weeks. During the course of treatment, the applicator may stay in place, or it may be put in place before each treatment. As with LDR implants, the applicator will be removed once treatment is finished.
Introduction to High Dose Rate Brachytherapy (HDR)
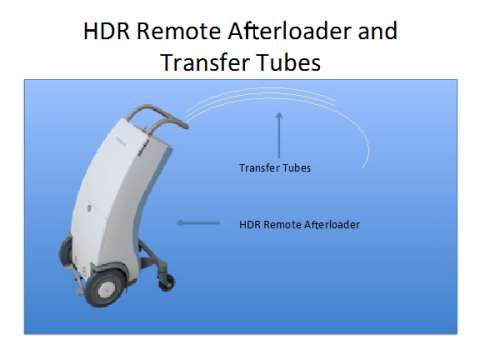
HDR is performed using a single tiny (1mm x 3 mm) highly radioactive source of Iridium-192 that is laser welded to the end of a thin, flexible stainless steel cable. The source is housed in a device called an afterloader. The computer-guided afterloader directs the source into the treatment catheters placed in and around the prostate by the brachytherapy physician. The source travels through each catheter in 5 mm steps, called "dwell" positions. The distribution of radiation and dose is determined by the dwell positions the source stops at and the length of time it dwells there. This ability to vary the dwell times is like having an unlimited choice of source strengths. This level of dose control is possible only with HDR.

HDR Treatement Process
- Step 1: Implant placement
The UCLA physicians decide which type of implant (intracavitary, intraluminal, or interstitial) the patient requires, based on location, tumor extent and other factors. - Step 2: Simulation
After the implant has been placed, either CT, MRI or special x-ray films are taken by the radiation therapists to determine the exact location of the implant in the body and the relationship to adjacent organs. These images assure that the implant and nearby organs are visualized clearly. The physician reviews these films and makes final adjustments to the implant if necessary. - Step 3: Dosimetry
The CT images or films are given to the dosimetrist to enter into the treatment planning computer. The computer does the initial calculation but it is the dosimetrist who "fine tunes" or customizes the radiation doses to conform to the target volume while minimizing the doses to the nearby normal tissues. After the treatment plan has been approved by the physician, the computer transfers the treatment plan instructions to the HDR remote afterloader. - Step 4: Treatment
The patient is moved into the brachytherapy treatment room. The ends of the applicator or treatment catheters that protrude outside the body are connected to "transfer" tubes which are then connected to the afterloader. The programmed instructions tell the afterloader where to direct the source and how long the source will stay in each dwell position. The patient is alone in the treatment room while the treatment is being given, but the therapists and nurses are continually monitoring the patient through an intercom and closed circuit TV monitors. The entire treatment process takes about 30-90 minutes depending on the size and complexity of the implant and the activity of the source. The actual radiation treatment itself takes approximately 5-15 minutes depending on the clinical situation. When the treatment is completed, the radiation source is retracted back into the HDR afterloader. There is no radiation left behind in the patient. Examples of various applicators and the Flexitron afterloader which is used at UCLA.
Examples of various applicators and the Flexitron afterloader which is used at UCLA. - Step 5: Implant Removal
After the treatment(s) have been given, the implant is removed. Intracavitary and intraluminal applicators are simple to remove and the patient goes home soon after removal. With interstitial implants, sutures holding the template and/or catheters in place are cut and the implant is gently removed. Some minor bleeding usually occurs, which is quickly stopped by applying direct pressure to the implant site with gauze pads. Post- implant skin care instructions are given by the nurses before the patient is discharged. A date for a follow-up appointment will also be given.
- Step 6: Follow-up
It is important that the patient keep us informed as to their recovery and any side effects. We pride ourselves on thorough patient follow-up, which is how we assess the efficacy of our HDR treatments and provides us with the data necessary in order to report our results in the medical literature.
Clinical Experience with HDR at UCLA
Our team at UCLA has some of the most clinical experience using brachytherapy for the treatment of all sites in the nation. We’ve safely delivered over 25,000 HDR treatments. Below is a table summarizing the types of cases that we’ve treated through March 2015. This table includes cases treated at CET as well as those treated since 2010 when CET moved to UCLA.
| UCLA and CET | Total Number of Implants |
|---|---|
| Prostate | 4570 |
| Breast | 290 |
| Gyn Interstitial | 1914 |
| Gyn Intracavitary | 3720 |
| Anal & Rectal Interstitial | 237 |
| H&N Interstitial | 546 |
| GI Intracavitary (Esophagus, Liver and Bile Duct) | 151 |
| Lung | 270 |
| Soft tissue Sarcomas | 27 |
| Others | 1081 |
| Total | 12806 |
| UCLA and CET | Total Number |
| Total Number Dosimetry Plans Performed | 14183 |
| Total HDR Treatment Delivered | 27270 |
| Total Implants Performed | 12806 |
*Statistics as of end of September 2016
Meet our Brachytherapy Team
Brachytherapy is a specialized skill and we've dedicated ourselves to building a team to take the best care of our patients as possible. Our team includes radiation oncologists, fellows, physician assistant, physicist, dosimetrist, nurses, radiation therapists, scrub tech, and the front office staff. There are only a few other Brachytherapy centers in the United States that commit this level of resource to caring for brachytherapy patients.
