Lumbar Stenosis
Find your care
At the UCLA Health Spine Center, our experts diagnose, manage and treat all spinal injuries and conditions. Call 310-319-3475 to connect with a spine specialist.
Fax: 424-259-6560
What You Should Know About Lumbar Stenosis
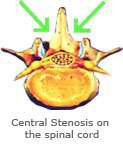
Lumbar stenosis results from the gradual wear and tear on the spine associated with aging. A normal process, the spinal canal is widely patent in our youth, but gradually becomes narrower as the surrounding bone, ligaments, and discs become thicker and encroach on the spinal nerves.
Symptoms
Unlike a lumbar disc herniation which can present acutely, lumbar stenosis is a slowly evolving degenerative phenomenon that takes many years to occur. As such, the onset of symptoms can be quite insidious, and not detected until the stenosis is fairly severe. The classic symptoms are leg pain that is worsened with standing and walking, and improved with sitting and/or lying down. Frequently patients will notice that while standing, their symptoms are lessened by leaning over a shopping cart or bending forward. This maneuver serves to further open the spinal canal and at least partially relieve the stenosis.

Diagnosis
The diagnosis of lumbar stenosis is confirmed using standard lumbar MRI and or CT/myelography.
Treatment
The initial treatment of lumbar stenosis can be nonoperative or operative, depending on severity of symptoms and patient and physician preference. Due to the chronic nature of disease, and degree of narrowing, nonoperative treatment tends to not be as successful as it is for lumbar disc herniation. Operative management commonly consists of removal of the offending bone, ligament and soft tissue that are causing the spinal canal narrowing, called a laminectomy. In cases where concerns of postoperative spinal instability may occur, such as spondylolisthesis, a simultaneous fusion may be recommended. Other surgical techniques include the placement of spinal spacers which open the spinal canal without the need for a laminectomy.