Re-do Parathyroid Surgery
Find your care
We deliver effective, minimally invasive treatments in a caring environment. Call 310-267-7838 to connect with an expert in endocrine surgery.
What is Re-do Parathyroid Surgery?
Re-do parathyroid surgery, also known as remedial or reoperative parathyroid surgery, is one of the most challenging aspects of managing parathyroid disease. It is defined as a subsequent operation to treat parathyroid disease, most often primary hyperparathyroidism, usually after the first operation has failed to achieve cure or the disease comes back after a period of time.
We also commonly see patients who have had two failed prior operations, and the highest number of prior failed operations we have seen in one patient has been seven.
Most patients with a history of prior failed parathyroid surgery can be cured with a re-do parathyroid operation. However, we must qualify this statement by adding that the risks of re-do parathyroid surgery are higher than that of initial surgery, and that re-do parathyroid surgery should only be performed in expert centers (there are only a handful of qualified centers in the nation). Indeed, most surgeons practicing outside of expert parathyroid surgery centers are (wisely) unwilling to perform re-do parathyroid surgery given its significant challenges.
How often is re-do parathyroid surgery necessary?
Unfortunately, quite often. Depending largely on surgeon experience, initial parathyroid surgery is unsuccessful in 1-30% of patients (see Parathyroid surgery success). As a result, we evaluate several patients in need of re-do parathyroid surgery every week and dedicate one full day per week to operating on patients who need re-do neck operations of various types. This work is laborious and fraught with risk. To state the obvious, it is highly preferable for patients to avoid the need for re-do parathyroid surgery altogether by having things done properly the first time. We will come back to this important theme later on.
Through our research, we have learned that only a small fraction (about 10%) of patients with failed initial parathyroid surgery ever undergo re-do surgery. For reasons that we do not fully understand, the majority of patients who are not cured during initial surgery are left to suffer the adverse health effects of primary hyperparathyroidism for the rest of their lives. Health problems associated with primary hyperparathyroidism include kidney stones, osteoporosis, abdominal pain, musculoskeletal pain, and fatigue (see Parathyroid surgery benefits). When UCLA Endocrine Surgery was established in 2006, we soon discovered that many local endocrinology practices were burdened with literally dozens of patients who had had failed parathyroid surgery. This motivated us to develop specific expertise and dedicated resources for this challenging group of patients. Over time, UCLA has become a destination medical center for patients who require re-do neck surgery; our patients come from throughout the Southern California metropolitan area, across the nation, and from overseas (see Distance surgery program).
Why does initial parathyroid surgery sometimes fail?
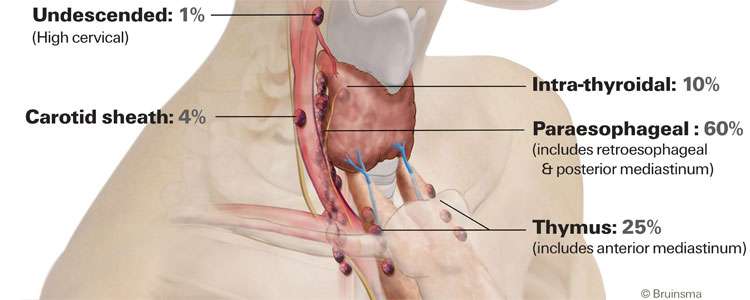
Causes of persistent hyperparathyroidism (failed initial surgery).
The reasons behind failed parathyroid surgery are complex, but the leading cause is surgeon inexperience. Our research has shown that, in order to achieve good outcomes, a surgeon should perform at least one parathyroid operation per month. In order to achieve superior outcomes, a surgeon should perform at least one parathyroid operation per week (see Parathyroid surgery success). At UCLA, we typically perform 8 parathyroid operations per day. The most common explanation for failed initial parathyroid surgery is missed adenoma, i.e. the surgeon was unable to locate the single abnormal parathyroid gland responsible for the patient's high blood calcium level. Less commonly, failed surgery may arise when the surgeon only removes one gland in a patient who has multiple abnormal parathyroid glands (missed double adenoma or missed hyperplasia).
Why does primary hyperparathyroidism sometimes come back after initial surgery appears successful?
Causes of recurrent hyperparathyroidism.
Recurrent hyperparathyroidism is defined by the re-appearance of high blood calcium levels more than 6 months after successful initial surgery for primary hyperparathyroidism. Potential causes of recurrent hyperparathyroidism are:
- Dormant (sleeping) second parathyroid adenoma, also known as subordinate adenoma. These patients have two abnormal parathyroid glands present at the time of their first operation. However, one of them, the dominant adenoma, is more active than the other one. The dominant adenoma releases more parathyroid hormone (PTH) and pushes the blood calcium to a high level, causing the subordinate adenoma to remain quiet. When the dominant adenoma is removed during initial surgery, the subordinate adenoma then "wakes up" and starts to overproduce PTH, leading to recurrent hyperparathyroidism. The solution to this problem is to remove the second adenoma.
- Missed parathyroid hyperplasia. This is when a single adenoma is removed in a patient who in fact has 4 abnormal parathyroid glands. The best operation for patients with parathyroid hyperplasia is a subtotal parathyroidectomy (removal of three and a half glands). The solution to the problem of missed parathyroid hyperplasia is complex: the re-operation must achieve removal of 2 and a half parathyroid glands. The entire medical literature contains only a small number of documented cases where this has been achieved. Read about how UCLA Endocrine Surgery has tackled the problem of missed parathyroid hyperplasia >
- Incomplete removal of a single parathyroid adenoma. In these cases, the first surgeon has cut across the abnormal parathyroid gland. The remaining portion then grows until the patient's PTH and calcium levels rise again, resulting in recurrent hyperparathyroidism. The solution is to go back and remove the abnormal parathyroid tissue, cleanly and entirely.
- Parathyromatosis. Parathyromatosis occurs when the initial surgeon breaks open the capsule of a parathyroid adenoma, causing abnormal parathyroid cells to spill out and seed the nearby soft tissues of the neck. This is one of the worst problems we encounter during re-operative parathyroid surgery. Often, the parathyroid tissue is seeded across a wide area of the neck, which makes parathyromatosis potentially incurable. During reoperation, it is frequently necessary to remove nearby muscle, fat, connective tissue, and thyroid tissue in order to achieve a wide excision. Even this may not bring about a durable cure, because a few small seeds left behind can eventually grow back.
- Parathyroid carcinoma. Parathyroid cancer is extremely rare, affecting less than 1 in 1000 patients with primary hyperparathyroidism. This is obviously a very serious problem which can be life-threatening. Sometimes it is hard to tell the difference between parathyroid carcinoma and parathyromatosis - this issue should be carefully analyzed by an expert pathologist and endocrine surgeon in cases where the exact diagnosis is uncertain.
When should re-do parathyroid surgery be considered?
The best candidate for re-do parathyroid surgery is a patient who (A) has severe or symptomatic primary hyperparathyroidism, and (B) has a clear target on imaging. This gets to the key question when planning any operation: What is the balance of risk and benefit? Patients with severe hyperparathyroidism (blood calcium level >11.5 mg/dL) and those with symptoms such as kidney stones, loss of kidney function, and osteoporosis have a strong motivation to pursue additional surgery. In other words, they have a lot to gain from being cured. We frequently will re-operate on patients with less severe disease, but this requires careful discussion between the patient, surgeon, and often the patient's endocrinologist.
When considering re-do parathyroid surgery, a clear target (or targets) on imaging is essential.
Why? During initial (first time) parathyroid surgery, the surgeon is able to move freely within the neck - healthy, previously untouched tissues are laid down in planes that separate easily during surgery and clearly show the underlying anatomy. During re-operation, scar tissue from initial surgery is present (to varying degrees) and makes dissection difficult. The surgeon is much less free to move around the neck; therefore, the best operation is an abbreviated one that focuses on a single known target or, in the uncommon case of missed hyperplasia, multiple targets.
What are the risks of re-do parathyroid surgery and how often is it successful?
Re-do parathyroid surgery is risky. Don't let anyone tell you otherwise. The risks are two to five times greater than for initial surgery. These risks include permanent hoarseness and failed surgery. In experienced hands, the risk of permanent hoarseness (recurrent laryngeal nerve injury) during initial parathyroid surgery should be less than 1 in 200. In re-do parathyroid surgery, the risk is 1-3%. Also, the second operation may not be successful. The success rate of initial parathyroid surgery by an expert surgeon is about 98%. The success rate of re-do parathyroid surgery by an expert surgeon is 80-95%.
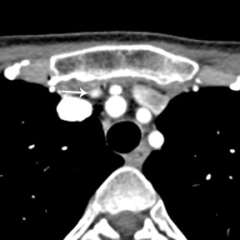
How do imaging results (scans) influence eligibility for re-do parathyroid surgery? The importance of parathyroid 4-D CT.
To a significant degree, re-do parathyroid surgery is driven by the presence of a clear anatomic target. Since 2012, UCLA Endocrine Surgery has employed parathyroid 4-D CT in the planning of all reoperations for primary hyperparathyroidism. [see video on parathyroid 4-D CT]. 4D-CT provides the highest possible anatomic detail and affords the highest likelihood of achieving a safe and successful second operation.
For us, 4D-CT technology has been a "game changer," enabling >95% of patients with failed initial operations to become eligible for reoperation, greatly aiding our ability to counsel patients on surgical strategy, and allowing us to complete reoperations in a much shorter time. Many patients are understandably disappointed and wary after their first parathyroid operation has failed. 4D-CT allows us to sit down with the patient and walk through a series of high-resolution images so that the patient and their family can get a clear understanding of the surgical plan.

What goes into planning re-do parathyroid surgery?
Re-do parathyroid surgery must be carefully planned. One should never rush into this type of operation, given its risks. We often meet patients who were rushed into a second operation elsewhere (sometimes only a day or two after initial surgery), and these reoperations almost universally fail. Planning for re-do parathyroid surgery involves a combination of detective work (analyzing what was done before) and assessing the patient's current state through laboratory testing (blood and sometimes urine) and imaging. We routinely request all prior operation reports, lab reports, pathology reports, and imaging reports. Also, we will request that all tissue samples (pathology slides) be sent to UCLA for re-analysis. The goal here is to question all the information associated with the first (failed) operation. Something clearly went wrong during initial surgery, and this is our chance to figure out what that was. This step of the process takes time, often several weeks while we work behind the scenes to scrutinize all of the records and microscopically analyze all of the tissues that were previously removed. Then, laboratory testing gives us information on the current severity of the patient's hyperparathyroidism. The last piece is imaging: 4D-CT is the cornerstone as you already know, and sometimes further imaging is required.
Where should re-do parathyroid surgery be performed and who should perform it?
Re-do parathyroid surgery should only be attempted by high-volume centers that specialize in parathyroid surgery. Only a small number of qualified centers exist.