Vertebroplasty / Kyphoplasty / Sacroplasty
Find Your Care
Our interventional neuroradiology team has paved the way for interventional procedures, creating several of the devices and techniques widely used today. Call 310-267-8761 to learn more about our services.

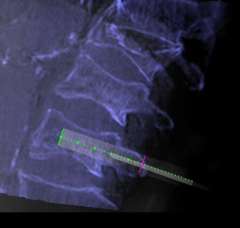
Compression fracture of the vertebral body is common. It is defined as a vertebral bone in the spine that has decreased in height by at least 15% due to the fracture (Figure 1). It is more common in the lower spine (thoracic and lumbar). Some vertebral compression fractures may heal on their own. However, in most cases, the compressed vertebrae do not fully heal since the fractured vertebral fragments continue to move even with a back brace.
Vertebral compression fractures can cause severe back pain leading to inability to perform daily activities, and potentially social isolation due to immobility. It is known, particularly in women, that vertebral compression fractures are associated with a 15% higher mortality than those without. In order to prevent this ripple effect, we can perform a minimally invasive percutaneous interventional procedure that can stabilize the fractured bone with the use of cement. Depending on the lesion, we offer 3 types of interventional procedures; vertebroplasty, kyphoplasty, and sacroplasty.
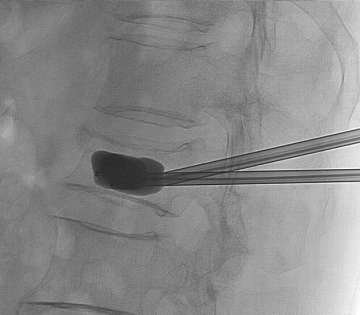
During the procedure, the patient is lightly sedated and lies on their tummy. Under x-ray guidance, we place the needle into the vertebral body (Figure 2). Unlike most pain services where a relatively simple portable C-arm X-ray machine is used, we use the state-of-the-art biplane neuro-angiosuite, which is capable of 3-D navigation in the brain and spine (Figure 3). In rare occasions, placement of the needle is challenging due to previous implantation of metal hardware that obscures the normal bony landmarks, or due to severe osteoporosis. The 3-D navigation capability provides us with the ability to very accurately place the needle without relying on the classic radiological bony landmarks (Figure 4).


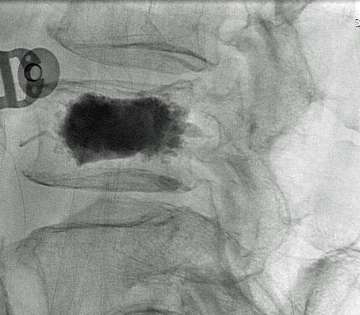
Once the needles are placed into the fractured vertebral body, cement is injected through the needles so that it can be stabilized from its inside (vertebroplasty).
If there is a need to restore the height of the fractured vertebral body, a balloon is inflated within the fractured vertebral body prior to cement injection (kyphoplasty / Figure 5). Once the bone cement hardens, it becomes an internal cast and completely stabilizes the lesion (Figure 6).
The patient can be discharged home the same day. In some cases, particularly after Kyphoplasty the patient may need to stay overnight. In our experience, more than 90% of the patients had complete disappearance or significant reduction of the pain over the next two weeks. For more detailed information, please feel free to contact us.