Prostate Cancer
Find your care
Our radiologists lead the way in prostate imaging. We offer the newest techniques to better detect and stage prostate cancer. Call 310-481-7545 to find out more about prostate imaging and treatment options.
About Prostate Cancer

Prostate cancer is the second most commonly diagnosed cancer in men (after skin cancer) and the second leading cause of cancer death in American men. However, screening with physical exam and the PSA blood test has shown only modest effects on mortality, such that the US Preventive Services Task Force recommends against screening with PSA. Recent studies in the New England Journal of Medicine showed no benefit for men with a PSA less than 10 ng/mL and no benefit to over treating men with low grade prostate cancer. Part of the problem is detecting cancer within the prostate, especially the high grade cancers, which are likely to grow and spread.
The current standard of care for men with an abnormal PSA or physical exam is systematic biopsies of the prostate that use ultrasound to identify the location of the prostate but not the individual cancers within it. This biopsy tissue is then evaluated by the pathologist under the microscope to decide if the abnormal appearance of the prostate glands suggests the presence of cancer. If present, the cancer severity is graded using the Gleason Score. However, biopsies are prone to error since they often detect low grade cancers with significant variability in detecting clinically important high grade cancers. Our experience and those of others suggests that an multi-parameteric MR scan may help detect and grade prostate cancers, separating the low grade from high grade variants. This can then lead to more targeted biopsies of suspicious high grade areas and in the future lead to localized treatment of these suspicious areas.
Detection, Diagnosis, and Staging
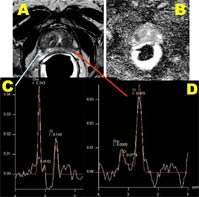
In addition to magnetic resonance imaging (MRI) and magnetic resonance spectroscopic imaging (MRSI), newer techniques such as diffusion weighted imaging and dynamic contrast enhanced perfusion imaging are being routinely used to better detect and stage prostate cancer and to assist surgeons in planning minimally invasive surgery and radiation oncologists in planning therapy. Diffusion imaging is a much faster technique which, although not as high resolution as conventional T2-weighted MRI, provides information on the degree of cellular crowding, which is worse in prostate cancer. Perfusion imaging has nearly the same fine detail as conventional T2-weighted MRI, but provides a map of blood flow, which is increased in cancer cells. These techniques have been proven at multiple high-powered academic institutions, including UCLA, to improve diagnostic accuracy.
These advanced preoperative imaging techniques enable surgeons to more accurately decide when to remove or spare the delicate neurovascular bundles in different cases. These decisions hold significant impact in patients' quality of life after surgery since urinary continence and sexual potency may be affected.
In some cases, the PSA blood test may suggest cancer but the biopsies fail to localize it, and the surgeon may not be able to feel the cancer with the DRE. In these cases UCLA can provide magnetic resonance imaging to biopsy the most suspicious area under direct MR guidance. Although MRI has not yet been shown to be an adequate substitute for biopsy, it can determine the likelihood that significant disease exists, and guide biopsy to ensure that no significant cancer is missed.
Prostate MRI: Diffusion and Spectroscopy
A: T2 Anatomic image
B: Applied diffusion coefficient
(tumor appears dark)
C: Abnormal spectroscopy
D: Normal spectroscopy

Perfusion Map - Perfusion map provides a map of blood flow, which is increased in cancer cells.
Treatment of Prostate Cancer
Treatment is determined primarily by whether the disease is localized or metastatic. Localized cancer is treated by surgery (radical retropubic prostatectomy or RRP), external beam or proton beam radiation therapy, implanted seed radiation, or, if not aggressive, active surveillance (watchful waiting). Metastatic prostate cancer is treated with androgen ablation (hormone) therapy.
Therefore, accurate staging of prostate cancer is important to choose an appropriate therapy. Currently, probability tables (nomograms) are used in clinical practice to determine whether prostate cancer is localized to the prostate or has extended beyond the gland (staging). MR imaging has been shown to improve accuracy of staging of prostate cancer in patients with intermediate or high probability of spread outside the gland.
At UCLA, conventional prostate magnetic resonance imaging (MRI) is supplemented by a variety of related functional MR techniques such as the technically demanding technique of magnetic resonance spectroscopic imaging (MRSI). MRSI is a MR technique that enables detection and quantification of normal and cancer related chemical compounds in the human prostate gland. Although normal human prostate contains large quantities of citrate and low levels of choline, prostatic cancer contains lower levels of citrate and high levels of choline. The first successful demonstration of 1H MR Spectroscopy in distinguishing a variety of chemicals such as citrate, choline, spermine and creatine in human prostate was demonstrated by Dr. Albert Thomas and colleagues at UCLA in 1990. (JMR 1990).UCLA is a leader in the development and implementation in magnetic resonance spectroscopic imaging of the prostate with a dedicated team of scientists, radiologists, and technologists with two decades of experience.