Meghan's Story: MS Care and New Treatments
Summer 2018
In the UCLA Department of Neurology, we strive to personalize treatment to the specific needs of each patient. This means that a traditional course of treatment for one patient may be ideal, but not right for another; or it might be the right treatment for a while, until a life event requires re-evaluation. Providing the right care means getting to know each patient and hearing his or her preferences. Guidelines in a neurological disease must take into account the individualized situations of the patients that experience this disease.
State of the art care of persons with Multiple Sclerosis (MS) mandates both highly individualized disease modifying therapy (DMT) and symptom management. Early and accurate diagnosis is key. Updated criteria now allow patients to be diagnosed after even a single episode or neurological symptom. Also, the integration of lifestyle, such as diet and exercise, along with traditional allopathic care is being recognized as increasingly important. New AAN guidelines provide detailed recommendations about the use of DMT in multiple sclerosis.
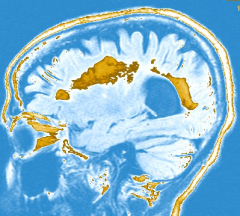
A Scenario: Meghan is a 22-year-old graduate student who is sent to the neurology office by the student health clinic with a chief complaint of pain and blurred vision in one eye. The neurological exam reveals decreased visual acuity in that eye and abnormal responses of the pupil to bright light. An MRI of the brain shows multiple lesions in the regions of the brain that carry connections, the cerebral “white matter.” In this MRI some of these lesions show enhancement with MRI contrast.
What is the course of action?
1. This patient should be placed on a vegan, gluten-free, paleo diet.
2. Treat the acute episode with steroids and then have a repeat MRI in 6 months.
3. Diagnose MS and proceed as in option #2
4. Diagnose MS and schedule another visit to discuss initiating a disease modifying treatment.
The most up-to-date guidelines are for option #4. This means that MS is a disease in which diagnostic tools are used, and treatments are initiated quickly. It is not a disease in which to idle around.
Another likely scenario: Meghan has been on DMT for about a year but she has had a clinically significant episode of gait imbalance, from which she made a good recovery. Her neurological exam is stable but her MRI shows new lesions in both brain and spinal cord.
What is the course of action?
1. Continue the current DMT and repeat MRIs every 3 months.
2. Change the DMT to another agent in the same class.
3. Change the DMT to a more effective or possibly more aggressive agent.
MS is a progressive disease, and one in which lifelong disability can accumulate. Yet, these new DMTs are not simple. They suppress the immune system’s attack on the brain, and require monitoring and close follow up. This can be a difficult balance but disability is a high price to pay. MS treatment guidelines suggest course of action #3.
And yet a third scenario: Meghan stabilizes clinically and in her MRI on a new DMT. She now wants to start a family.
What is the course of action?
1. Pregnancy is not advised for women with MS.
2. Pregnancy is not contraindicated but she should stop the DMT for an appropriate time period prior to conception.
3. She should remain on DMT up to and during pregnancy.
4. Breast feeding will increase the chance of a post-partum exacerbation.
The medical evidence and MS treatment guidelines recommend option 2. This requires close partnership between the patient and the MS doctor, and the specialized experience of a center like the UCLA Neurology Multiple Sclerosis Program.