In 2019, after the cancer in Lazaro Barajas’ colon spread to other organs and he progressed through chemotherapy options, doctors at UCLA Health deemed him a candidate for standard immunotherapy. It seemed to be working, until a few months later, his stage 4 metastatic colorectal cancer developed resistance to the drugs.
Seemingly out of options, Barajas then received potentially life-saving news from his treatment team: He could enroll in a clinical trial testing the safety and efficacy of a novel combination immunotherapy that would help his immune cells attack the cancer that had evaded the previous therapy.
Three years later, the clinical trial — along with a unique type of precision radiotherapy — has given the 43-year-old a new lease on life.
“He was told twice that he was going to die. When he didn’t respond to traditional immunotherapy, there was a significant worry that nothing was left for him,” says Sidharth Anand, MD, assistant professor and head of quality improvement for the Division of Hematology-Oncology, Department of Medicine, at the David Geffen School of Medicine at UCLA. Dr. Anand is a co-investigator on the trial led by Zev Wainberg, MD, a professor in the Division of Hematology-Oncology.
“(Barajas’) case shows that clinical trials really can make a difference,” Dr. Anand says.
Inhibiting immune checkpoints
While the immune system offers a powerful defense against foreign invaders, it also has a complex system of checks and balances. These “brakes,” or checkpoint molecules, prevent immune cells from overreacting and attacking healthy tissue.
Cancer cells can take advantage of those checkpoints, tricking the immune system into pumping its own brakes, which prevents it from launching an attack on tumors. By binding their surface proteins with the surface proteins of immune cells, cancer cells essentially flip the immune system’s “off” switch, Dr. Anand says.
Immunotherapy drugs, or checkpoint inhibitors, work by blocking tumor cell proteins from binding with T-cell proteins. This prevents the “off” signal from being activated and allows the immune system to recognize the cancer cells as dangerous threats.
One protein found on tumor cells that acts like a brake is called PD-L1, which binds with the PD-1 protein on T cells. During Barajas’ first round of immunotherapy, he was given a combination of drugs that blocked the checkpoint proteins (PD-1) from binding with their partner proteins (PD-L1). He was also given a drug that blocked the binding of another T-cell protein called CTLA-4.
Despite an initial response to these therapies, eventually, Barajas developed resistance to the drugs. This can happen for a variety of complex reasons, which is why researchers are constantly trying to develop and test new checkpoint inhibitors in clinical trials.
UCLA Health doctors put Barajas in a clinical trial that would test the experimental drug tiragolumab in combination with atezolizumab. Atezolizumab is already approved by the U.S. Food and Drug Administration to treat certain types of cancers.
While atezolizumab works by binding with PD-L1, the monoclonal antibody tiragolumab binds to a different inhibitory immune checkpoint, called TGIT. The TGIT checkpoint is distinct from, but complementary to, the PD-L1/PD-1 pathway, according to Dr. Anand. By inhibiting two different “brakes” in the immune system, this pair of drugs work together to turn the body’s surveillance system back on.
All of Dr. Anand’s patients with colorectal cancer undergo a series of tests to check for mismatch repair (MMR) deficiency or microsatellite instability (MSI-High). Tumors with mismatch repair deficiency or microsatellite instability can benefit from immunotherapy. What made Barajas a good candidate for immunotherapy is that his cancer cells had high microsatellite instability.
Dr. Anand says that unlike in Barajas’s case, 95% of colorectal cancer cases are classified as microsatellite stable (MSS). Patients with MSS colon cancer are typically unresponsive to immunotherapy.
“The majority of colorectal patients we see have MSS tumors. So, how do we get those patients’ immune systems to respond to therapy?” Dr. Anand says. “That’s really the holy grail we’re looking for.”
‘Spot treatment’
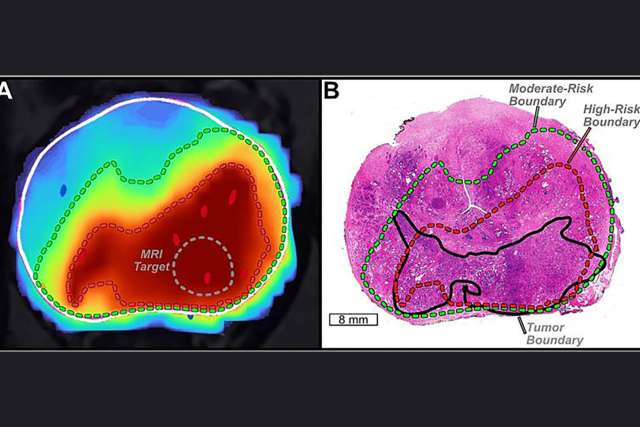
While the experimental immunotherapy succeeded in controlling Barajas’ cancer, the patient faced a setback in 2021 when scans showed cancer progression at some lymph nodes near the left groin and left pelvic region. His oncology team referred him to Michael Xiang, MD, PhD, a radiation oncology specialist and medical director of Santa Clarita Radiation Oncology.
To treat his oligoprogressive disease — the term used to describe a few areas of tumor growth in patients whose cancer is otherwise well-controlled — Dr. Xiang used stereotactic body radiation therapy (SBRT) as a kind of “spot treatment.”
SBRT delivers high doses of radiation to a highly targeted area in a short number of sessions, typically three to five.
“It’s a very precise and condensed treatment aimed at minimizing side effects and sparing the surrounding normal tissues and organs,” Dr. Xiang says.
SBRT is a relatively common treatment offered at most cancer centers. But in Barajas’ case at UCLA, Dr. Xiang and his radiation oncology team were able to offer the patient a much more personalized approach to his care.
With standard radiotherapy, each patient must undergo a scan in which clinicians map out exactly where the tumor and surrounding anatomy are located in the body. However, this process often offers a less-than-perfect guide by the time the patient is ready for radiation.
“The reality is that our internal anatomies are changing day to day, sometimes even minute to minute. Our bowels are moving, our bladder is filling and emptying,” Dr. Xiang says. “The traditional paradigm of radiation treatment is not able to adjust for those day-to-day variations in anatomy.”
But now, Dr. Xiang can offer patients like Barajas something called adaptive radiation therapy, which gives radiation oncologists a real-time view into the human body to adapt to the patient’s changing anatomy with high precision.
Dr. Xiang says “redrawing” the patient’s internal anatomy can be labor-intensive for the medical team and time-consuming for the patient, even with the aid of artificial intelligence. The adaptive treatment is therefore used on a case-by-case basis.
“You can think of it more as a special spice that you might take out of the cabinet when your dish really needs that special kick, and not something you’re adding to every single dish,” he says.
After adaptive SBRT treatment, scans showed the tumor areas in Barajas’ pelvis had decreased in size, demonstrating a good response to radiation. Also, his tumor marker (called CEA), which had been elevated and rising prior to treatment, dropped and returned to the normal range. Barajas continues on his clinical trial, which is keeping his overall disease in check.
Patients with colorectal or any other cancer type must work with their cancer team to develop a personalized approach to their specific disease, Dr. Anand says.
“We guide our patients’ treatments based on the degree of metastatic spread they have had, what driver mutation profile their tumors exhibit, the cadence of their disease, potential resistance mechanisms that may be in play, as well as their performance status,” he says.
“UCLA continues to identify novel pathways, as well as targeted treatments, that can help trigger the ability for the immune system to recognize, attack and kill cancer.”
Lauren Ingeno is the author of this article.