Alexandra Keir’s earliest memories include regularly receiving anesthesia and spinal taps on her lower back at the hospital.
At just two years old, Keir was getting chemotherapy for acute lymphoblastic leukemia (ALL), a rapidly progressing blood and bone marrow cancer. She recovered and reached the five-year cancer-free survival deadline, a timespan that usually assures survivors that their cancer will not relapse.
But at age 7, Keir was diagnosed again. This time it was with Ewing sarcoma, a cancer that occurs in the bones or surrounding soft tissue. She dealt with another round of treatment that included chemotherapy and radiation, and she recovered once more.
Seven years later, at 14, Keir developed cancer for the third time. She was diagnosed with spindle cell sarcoma, a rare bone cancer that affects the arms or legs. She underwent surgery and radiation – and recovered.
“I was diagnosed and treated for three different cancers before I entered high school,” Keir said.
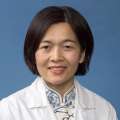
Now 27, the fourth-year student at the David Geffen School of Medicine at UCLA remains motivated by her grueling journey to become, and stay, cancer-free. She plans to work in pediatric cancer research and improve survival rates for childhood cancers, as well as provide holistic care.
“My current path,” she said, “allows me to create something meaningful from my history.”
A rare case
ALL is the most common type of blood cancer in children, according to the National Cancer Institute. With current treatment protocols, more than 85-90% of children with standard risk ALL survive without relapse.
While Keir’s subsequent second cancer was not a relapse, her diagnosis of Ewing sarcoma was still rare. It was so rare, her doctor published a case report concluding that her tumor developed sporadically, and was unrelated to her previous cancer treatment.
Keir’s long-term survival is fortunate, said Steven J. Jonas, MD, Ph.D., a pediatric hematology oncology physician scientist who is collaborating with her on a research project.
It progressively gets harder to treat subsequent cancers, he said. “There is a certain limit for the types of chemotherapy and toxicity that your body is able to withstand over the course of life.”
Depending on the type of cancer a pediatric patient has and the treatments they receive, long-term side effects may include stifled bone growth, fertility issues or chronic heart issues.
At worst, treatment may the increase the risk of secondary cancers because it damages healthy cells, too. According to Keir’s pediatric oncologist, Keir’s third diagnosis of spindle cell sarcoma may have been caused by the high doses of radiation used to treat her Ewing sarcoma.
“Understanding these associations – and screening for late effects like secondary cancers – is a big part of long-term cancer survivorship care that patients like Alex receive,” Dr. Jonas said.
Path to medical school
Keir’s early exposure to clinicians planted a seed in her to pursue a career in health care. After all, she felt like the hospital was her second home. But it was not until she was exposed to clinical research and excelled in her upper-division coursework as an undergrad at UCLA that she believed in her capabilities to become a doctor, she said.
“By that point, I actually believed that I could do medicine well, and realized that’s what I wanted,” Keir said.
Working with kids and families affected by cancer in the volunteering and fundraising worlds reaffirmed that decision. Keir volunteered for UCLA Mattel’s Child Life program, where she played games with pediatric patients, and became an ambassador for Alex’s Lemonade Stand Foundation, an organization dedicated to funding pediatric cancer research and supporting families affected by their child’s disease.
“The foundation helps parents and the siblings who are very affected, sometimes even more affected, than the child themselves,” Keir said. “They’re often ignored in fundraising efforts because they're not the primary focus.”
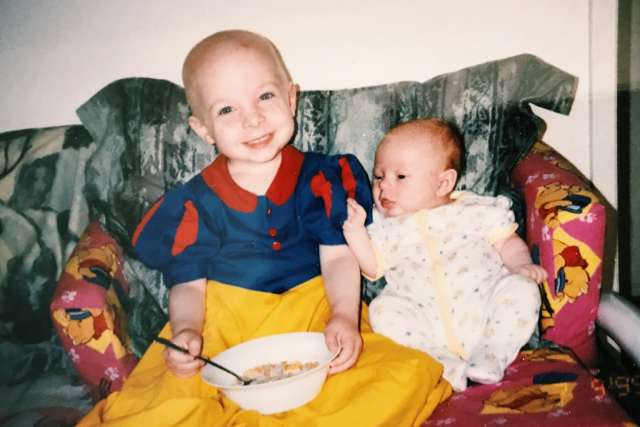
Keir’s cancer experiences were difficult for her parents because they understood more deeply how different her life was when compared to other children. It was at her third diagnosis that Keir felt the full emotional weight of her experiences.
Keir said she did not want to pursue aggressive treatment if it was not going to cure her disease when it initially looked like a relapse. Her parents fully supported this decision.
The treatment, which involved surgery and six weeks of radiation, “was my most straightforward,” she said. “But it was the most difficult for me to get through, emotionally.”
Contributing to the research
Treatment for pediatric cancers have overall made strides in the past 30 to 50 years in terms of survival rates, according to Keir. Standard risk ALL is approaching a 95% 5-year survival rate, for example.
The same cannot be said for Ewing sarcoma, which has a 60-70% 5-year survival rate. This drops in half with evidence of relapsed, metastatic disease, or disease progression. Basic Ewing sarcoma chemotherapy has also not changed since the 1900s.
Closing the gap in survival outcomes between those two cancers is one of the reasons Keir would like to pursue a specialty in pediatric hematology oncology – and she has already made her mark in the research and clinical setting.
During medical school, Keir began working with the UCLA Pediatric Bone and Soft Tissue Sarcoma Program under the mentorship of Dr. Jonas and Noah Federman, MD, the Nancy and Jonathan Glaser family endowed chair for pediatric sarcomas and health sciences professor of pediatrics and orthopedic surgery. There, she set up a clinical workflow that involved meeting Ewing sarcoma patients and getting their consent to donate blood samples for research.
“Keir understands what patients and families are going through and connects with these folks in a way not very many people can do,” Dr. Jonas said.
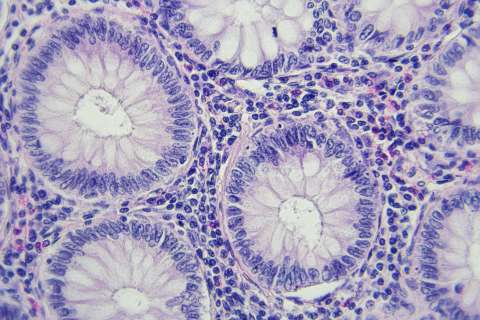
Dr. Jonas and his colleagues are developing liquid biopsy diagnostic tools that use nanotechnologies to monitor how pediatric cancers respond to treatments, with the ultimate goal of modifying cancer treatment plans in real-time. The project is a collaboration with Hsian-Rong Tseng, Ph.D., professor of molecular and medical pharmacology, and Yazhen Zhu, MD, a research pathologist and assistant professor at DGSOM.
“If a liquid biopsy indicates everything is going well, it might be possible to pull back on treatment and save patients from the toxicity that they still, unfortunately, have to face with current cancer treatments like chemotherapies,” Dr. Jonas said.
“If the liquid biopsy reveals signs that the treatment isn’t working, maybe that gives an oncologist an indicator of when they might have to step on the gas a little bit more and/or change up the punch.”
The blood samples Keir had collected were used to test the nanotechnology-enabled platform. Keir also analyzed and evaluated data from the project.
She is a coauthor on research that this lab has published demonstrating their method, and has received a training grant from Alex’s Lemonade Stand to continue her work.
Holistic care
Beyond working in research, Keir is interested in providing holistic care to pediatric patients during and after treatment.
Psychological care was not largely accessible or available at the time Keir went through any of her diagnoses. She also did not know where to look for cancer-specific resources that help patients with the aftermath of their disease.
While Keir says that mental and emotional health resources have become more available for pediatric cancer patients since she was a patient, she would like to pair pediatric patients and their families with psychological and recreational resources.
As a fourth-year medical student, Keir is currently applying for a pediatric residency. After completing residency, she plans to apply for a fellowship in pediatric hematology oncology.
“I hope to serve as a role model for what a positive, happy, and healthy life can look like after a devastating diagnosis,” Keir said.
“After challenging years, life can be meaningful.”