Oxidized lipids are known to play a key role in inflaming blood vessels and hardening arteries, which causes diseases like atherosclerosis. A new study at UCLA demonstrates that they may also contribute to pulmonary hypertension, a serious lung disease that narrows the small blood vessels in the lungs.
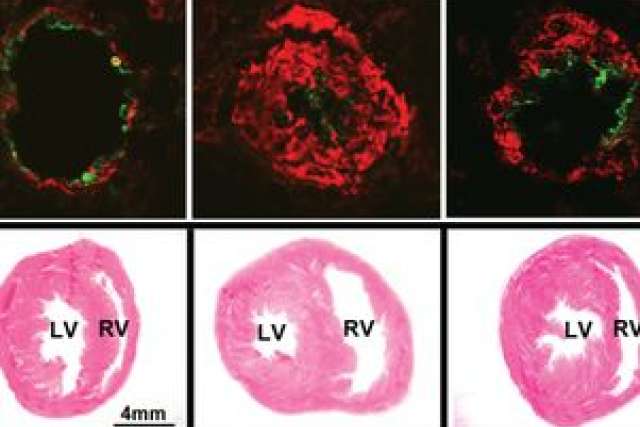
Using a rodent model, the researchers showed that a peptide mimicking part of the main protein in high-density lipoprotein (HDL), the so-called “good” cholesterol, may help reduce the production of oxidized lipids in pulmonary hypertension. They also found that reducing the amount of oxidized lipids improved the rodents’ heart and lung function.
The study appears in the current online edition of the peer-reviewed journal Circulation.
A rare progressive condition, pulmonary hypertension can affect people of all ages. The disease makes it harder for the heart to pump blood through these vital organs, which can lead to heart failure.
“Our research helps unravel the mechanisms involved in the development of pulmonary hypertension,” said Dr. Mansoureh Eghbali, the study’s senior author and an associate professor of anesthesiology at David Geffen School of Medicine at UCLA. “A key peptide related to HDL cholesterol that can help reduce these oxidized lipids may provide a new target for treatment development.”
Lipids such as fatty acids become oxidized when they are exposed to free radicals — tiny particles that are produced when the body converts food into energy — or when they are exposed to pollution, and in numerous other ways.
UCLA
Dr. Mansoureh Eghbali
Although researchers have known that oxidized lipids played a role in the development of atherosclerosis and other vascular diseases, the UCLA team discovered higher-than-normal levels of oxidized proteins in rodents with pulmonary hypertension.
The UCLA researchers also knew that apoA-1, a protein that is a key component of HDL cholesterol, can reduce oxidized lipids, so they used a small peptide called 4F that mimics the action of apoA-1 and found that the 4F not only decreased the levels of oxidized lipids in the rodents, but also improved their heart and lung function. Specifically, the peptide restored the altered expression of a key molecule called micro ribonucleic acid (microRNA-193), which targets the action of essential enzymes involved in the production of oxidized lipids.
“The increased amounts of these oxidized lipids due to pulmonary hypertension keeps the expression of this molecule under check, which aggravates symptoms of the disease,” said first author Dr. Salil Sharma, a UCLA postdoctoral researcher in anesthesiology.
By restoring the expression of microRNA-193 to its full potential, the researchers reduced the amount of oxidized lipids in the animals with pulmonary hypertension.
One of the hallmarks of pulmonary hypertension is a proliferation of smooth muscle cells in the lungs, which is harmful because it narrows the lungs’ small blood vessels.
Additionally, Eghbali’s team found reduced levels of microRNA-193 in the blood and lung tissue of human patients with the disease and discovered that they could slow the proliferation of the smooth muscle cells by increasing levels of microRNA-193 in the cells that had been isolated from these patients’ lungs.
Further research will be required to test the potential of the HDL-related peptide and microRNA-193 in human disease, and to better understand how the levels of oxidized lipids in the blood may correlate to disease severity in people with pulmonary arterial hypertension.
The study was funded in part by the American Heart Association, the National Institute of Health, the UCLA Clinical and Translational Science Institute and the Iris Cantor–UCLA Women’s Health Center executive advisory board.
The study’s other authors were Dr. Soban Umar, Andrea Iorga, Gabriel Wong, Denise Mai and Dr. Kaveh Navab of the division of molecular medicine at UCLA’s department of anesthesiology; David Meriwether, Dr. Mohamad Navab, Dr. Alan Fogelman and Dr. Srinivasa Reddy of the division of cardiology at UCLA’s department of medicine; Dr. David Ross of the division of pulmonary critical care medicine at the David Geffen School of Medicine at UCLA’s department of medicine; and Francois Potus, Sandra Breuils-Bonnet, Dr. Steve Provencher and Dr. Sébastien Bonnet of Laval University in Québec, Canada
All of the intellectual property for the HDL-related peptide is owned by the University of California Regents and managed by the UCLA Office of Intellectual Property and Industry Sponsored Research. The technology is currently licensed exclusively to Bruin Pharma Inc. Fogelman, Navab and Reddy are principals in Bruin Pharma, and Fogelman is an officer in the company. Other disclosures are listed in the manuscript.