A team of researchers and clinicians from UCLA’s Jonsson Comprehensive Cancer Center and the California Institute of Technology (Caltech) has published the first proof that a targeted nanoparticle—used as an experimental therapeutic and injected directly into a patient’s bloodstream—can navigate into tumors, deliver double-stranded small interfering RNAs (siRNAs) and turn off an important cancer gene.
Moreover, the team provided the first demonstration that this new type of therapy can make its way to human tumors in a dose-dependent fashion, meaning a higher number of nanoparticles sent into the body results in a higher number of nanoparticles found in the tumor cells.
Published in the March 21, 2010 advance online edition of the journal Nature, the results demonstrate the feasibility of using both nanoparticles and RNA interference (RNAi)-based therapeutics in patients. The study also opens the door for future “game-changing” therapeutics that attack cancer and other diseases at the genetic level, said Mark E. Davis, the Warren and Katharine Schlinger Professor of Chemical Engineering at Caltech and the research team’s leader.
The discovery of RNA interference, the mechanism by which double strands of RNA silence genes, won researchers Andrew Fire and Craig Mello the 2006 Nobel Prize in Physiology or Medicine. The scientists first reported finding this novel mechanism in worms in a 1998 Nature paper. Since then, the potential for this type of gene inhibition to lead to new therapies for diseases like cancer has been highly touted.
RNAi is a new way to stop the production of proteins, researchers said. What makes it such a potentially powerful tool is that its target is not a protein. The vulnerable areas of a protein may be hidden within its three-dimensional folds, making it difficult for many therapeutics to reach. In contrast, RNA interference targets the messenger RNA (mRNA), which encodes the information needed to make a protein.
“In principle, that means every protein now is druggable because its inhibition is accomplished by destroying the mRNA,” Davis said. “And we can go after mRNAs in a very designed way given all the genomic data that is and will become available.”
Still, there have been many potential roadblocks to applying RNA interference technology in humans. One of the most problematic has been finding a way to ferry the therapeutics, made up of fragile siRNAs, into tumor cells after injection into the bloodstream. Researchers, however, found a solution. Even before the discovery of RNAi, Davis and his team had begun working on ways to deliver nucleic acids into cells via systemic administration. They eventually created a four-component system featuring a unique polymer that can self-assemble into a targeted, siRNA-containing nanoparticle.
“These nanoparticles are able to take the siRNAs to the targeted site within the body,” Davis said. “Once they reach their target—in this case, the cancer cells within tumors—the nanoparticles enter the cells and release the siRNAs.”
The scientific results described in the Nature paper are from a Phase I clinical trial at UCLA’s Jonsson Comprehensive Cancer Center and a site in Texas that began treating patients with the nanoparticles in May 2008. Phase I trials are, by definition, safety trials. They are designed to determine dose level and toxicity. Phase I trials can also provide an in-human scientific proof of concept—which is what is being reported in the Nature paper.
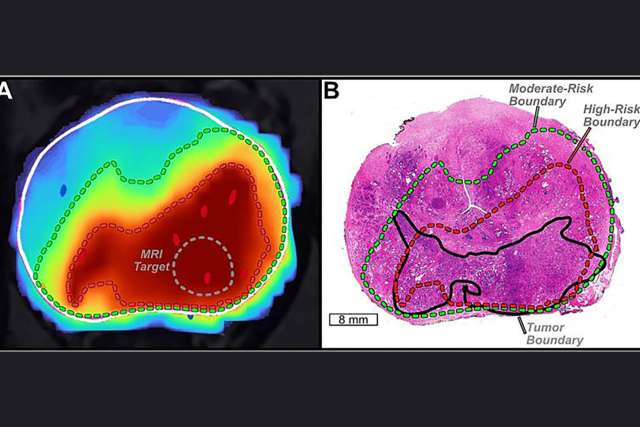
Using a new technique developed at Caltech, the team was able to detect and image nanoparticles inside cells biopsied from the tumors of several study participants. In addition, Davis and his colleagues were able to show that the higher the nanoparticle dose administered to the patient, the higher the number of nanoparticles found in tumor cells—the first example of dose-dependent response using targeted nanoparticles.
Even better, Davis said, the results showed the siRNAs had done their job. In the tumor cells analyzed by the researchers, the mRNA encoding the cell-growth protein ribonucleotide reductase had been degraded. This degradation, in turn, led to a loss of the protein that was driving cancer growth.
Additionally, the mRNA fragments found were the exact length and sequence they should have been if they'd been cleaved in the spot targeted by the siRNA.
“It's the first time anyone has found an RNA fragment from a patient's cells showing the mRNA was cut at exactly the right base via the RNAi mechanism,” Davis said. “It proves that the RNA interference mechanism can happen using siRNA in a human.”
“There are many cancer targets that can be efficiently blocked in the laboratory using siRNA, but blocking them in the clinic has been elusive," said Dr. Antoni Ribas, associate professor of medicine and surgery, and a researcher at UCLA's Jonsson Comprehensive Cancer Center who is senior author of the study.
“This is because many of these targets aren't amenable to be blocked by traditionally designed anti-cancer drugs,” said Ribas, who ran the Phase I clinical trial. “This research provides the first evidence that what works in the lab could help patients in the future by the specific delivery of siRNA using targeted nanoparticles. We can start thinking about targeting the untargetable.”
Although this is very early data and more research is needed, researchers characterized the study as promising.
The Phase I trial was sponsored by Calando Pharmaceuticals, a Caltech startup.
Study Provides Proof in Humans of RNA Interference Using Targeted Nanoparticles

Dr. Antoni Ribas is director of the UCLA Health Jonsson Comprehensive Cancer Center's tumor immunology program and president of the American Association for Cancer Research.
Related Content
Articles:
Services:
Physician
Related Articles
December 12, 2025
5 min read
December 11, 2025
4 min read
December 11, 2025
3 min read