Scientists from the UCLA Jonsson Comprehensive Cancer Center and Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research are bringing stem cell science directly to cancer patients with an exciting new clinical trial scheduled to begin in early 2014. Drs. Dennis Slamon and Zev Wainberg are recipients of the Disease Team Therapy Development III Award, a grant funded by the California Institute of Regenerative Medicine (CIRM), the state stem cell agency. Slamon and Wainberg’s phase I clinical trial will test a new drug that targets cancer stem cells and has been approved to begin enrolling patients in the U.S. and Canada.
The announcement of the award came on December 12, 2013 at the meeting of the CIRM Independent Citizen’s Oversight Committee (ICOC) at the Luxe Hotel in Los Angeles.
The project builds on Slamon’s previous work, partially funded by CIRM, to develop a drug that targets tumor initiating cells, that was conducted with Wainberg, also assistant professor of hematology/oncology at UCLA, and Dr. Tak Mak, director, Campbell Family Institute of the University Health Network in Toronto, Canada.
Slamon, renowned for his research that led to the development of Herceptin, the first FDA-approved targeted therapy for breast cancer, is the director of clinical and translational research at the UCLA Jonsson Comprehensive Cancer Center, and professor, chief and executive vice chair for research in the division of hematology/oncology.
With investigational new drug approval from the Food and Drug Administration (FDA) and Health Canada, the Canadian government’s therapeutic regulatory agency, this trial is an international effort to bring leading-edge stem cell science to patients.
“We are delighted to receive this CIRM grant that will drive our translational research from the laboratory to the clinic,” Slamon said. “It will allow us to test our targeted drug in a phase I clinical trial.”
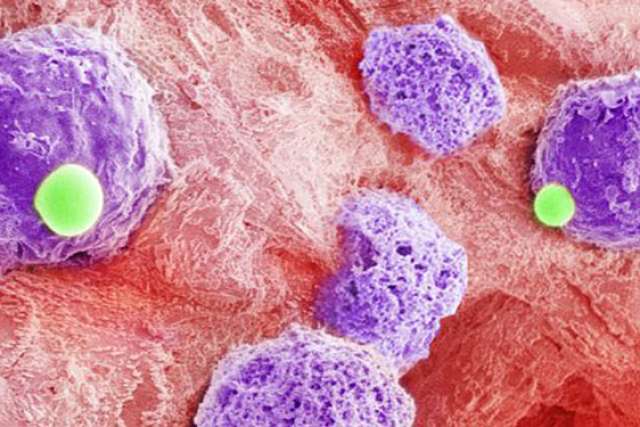
The trial is based on the evidence built over the last decade for what has become known as the cancer stem cell hypothesis. According to this hypothesis, cancer stem cells are the main drivers of tumor growth and are also resistant to standard cancer treatments. One view is that cancer stem cells inhabit a “niche” that prevents cancer drugs from reaching them. Another view is that tumors can become resistant to therapy by a process called cell fate decision, by which some tumor cells are killed by therapy and others become cancer stem cells. These cancer stem cells are believed to be capable of self-renewal and repopulation of tumor cells, resulting in the recurrence of cancer.
The target of the new drug is an enzyme in cancer stem cells and tumor cells called Polo-like kinase 4, which was selected because blocking it negatively affects cell fate decisions associated with cancer stem cell renewal and tumor cell growth, thus stopping tumor growth.
This potential anti-cancer drug is now ready to be tested in humans for the first time. “Our goal is to test this novel agent in patients in order to establish safety and then to proceed quickly to rapid clinical development,” said Wainberg. “We are excited to continue this academic collaboration with our Canadian colleagues to test this drug in humans for the first time.”
Drs. Slamon, Wainberg, Mak and colleagues will also look for biological indications, called biomarkers, that researchers can use to tell if and how the drug is working.